
Click on graphic above to navigate the 165+ web files on this website, a regularly updated Gazetteer, an in-depth description of our island's internally self-governing British Overseas Territory 900 miles north of the Caribbean, 600 miles east of North Carolina, USA. With accommodation options, airlines, airport, actors, actresses, aviation, banks, beaches, Bermuda Dollar, Bermuda Government, Bermuda-incorporated businesses and companies including insurers and reinsurers, Bermudians, books and publications, bridges and causeway, charities, churches, citizenship by Status, City of Hamilton, commerce, communities, credit cards, cruise ships, cuisine, currency, disability accessibility, Devonshire Parish, districts, Dockyard, economy, education, employers, employment, environment, executorships, fauna, ferries, flora, former military bases, forts, gardens, geography, getting around, golf, guest houses, highways, history, historic properties, Hamilton, House of Assembly, housing, hotels, immigration, import duties, internet access, islands, laws, legal system and legislators, main roads, marriages, media, members of parliament, money, motor vehicles, municipalities, music and musicians, newcomers, newspaper, media, organizations, parks, parishes, Paget, Pembroke, performing artists, residents, pensions, political parties, postage stamps, public holidays, public transportation, railway trail, real estate, registries of aircraft and ships, religions, Royal Naval Dockyard, Sandys, senior citizens, Smith's, Somerset Village, Southampton, St. David's Island, St George's, Spanish Point, Spittal Pond, sports, taxes, telecommunications, time zone, traditions, tourism, Town of St. George, Tucker's Town, utilities, water sports, Warwick, weather, wildlife, work permits.
By Keith Archibald Forbes (see About Us).

![]()
 Healthcare in Bermuda is
mandatory and the world's most expensive
Healthcare in Bermuda is
mandatory and the world's most expensiveMore so than even in the USA, especially from June 1, 2019 after new Bermuda Government charges. Bermuda's Members of Parliament have approved a succession of significant rises in hospital fees in recent years.
All visitors to Bermuda from all countries by sea or air, on vacation or business or coming to see family or friends, should protect themselves in their home countries against any medical contingency they may incur while they are in Bermuda. For any unforeseen medical emergencies or unexpected death while in Bermuda, they should take out adequate travel/health and major medical insurance coverage before they arrive. They do not qualify for any type of contributory Bermuda health insurance coverage offered to qualifying locals.
Although Bermuda is a British Overseas Territory, it offers no reciprocal health services for travelers, (as happens until December 31, 2929 between the United Kingdom and countries in the European Community). There are no reciprocal healthcare arrangements with the USA, Canada, United Kingdom or any other country. However, if a visitor from the USA is hospitalized while in Bermuda and has appropriate and valid Blue Cross/Blue Shield insurance, the King Edward VII Memorial Hospital will likely accept that as insurance coverage, upon confirmation of insurability.
Annual average spending on health coverage in Bermuda in 2019 by individuals was more than $11,952, the highest in the world. See the Bermuda Health Council release of its last National Health Accounts Report, showing an increase in per capita health spending of almost 60 per cent over the six-year period. The document reveals that health expenditure on the Island does not compare well in terms of affordability to the 34 countries in the Organization for Economic Co-operation and Development (OECD). Health spending in Bermuda reached 13 percent of the country’s gross domestic product (GDP) — compared with the OECD average elsewhere of 9.3 per cent
Unlike Affordable Healthcare (Obamacare) which began in the USA on October 2013 and despite the change in the US Presidency since then still has an average price of under $400 a month in all 50 states, there has never been anything similar in Bermuda. Employers, not employees, choose health insurance for the employer and its employees initiating or dropping coverage, or picking among such options as monthly premium costs, co-payments, annual deductibles and prescription drug coverage and what the latter includes or excludes. Employees cannot opt out of an employers health insurance coverage. However, employer's participating insurance companies cannot turn employees away or charge them more because they have an illness or medical condition. But if an employee has a qualifying "event" (such as getting married or divorced or having or adopting a child, or if a hitherto-unemployed spouse or child becomes employed, as two examples), he or she can change the insurance coverage to include a non-working spouse and exclude a working spouse..
There is no Long Term Health Care Insurance offered at all by local insurance companies. And those many major international insurance companies that have incorporated in Bermuda to minimize their tax liabilities in other countries where they operate freely and do offer Long Term health care insurance are not allowed to do so in Bermuda to Bermuda residents under Bermuda laws.
Many residents who are retirees, whose major medical insurance through their employers stops when they reach 65, have to spend thousands of dollars yearly locally for post-retirement health, hospital, major medical and prescriptions insurance from their savings.
Bermuda's medical facilities are good for a 21-square mile island but not equipped for very serious conditions, such as heart, stroke and other conditions. If you require extensive and/or intensive treatment you will likely be air-lifted elsewhere, usually to good hospitals in the USA, possibly Lahey in Boston or Johns Hopkins in Baltimore or New York or Philadelphia, at your expense. All medical doctors in Bermuda must be licensed locally before they qualify and - except for those in the public sector working at a hospital - all are private.
Some pharmaceuticals available without prescription elsewhere require prescriptions in Bermuda from registered local medical doctors. Not all drugstores in Bermuda are licensed dispensing pharmacies.
While in Bermuda, if they need any hospital or medical attention or services they must be paid for in cash or by credit card. No personal checks will be accepted. Costs are in accordance with the scale of charges in effect from King Edward VII Memorial Hospital (KEMH) and local medical practitioners. The Bermuda Hospitals Board (Hospital Fees) Regulations state what they are currently. KEMH is Bermuda's only Accident and Emergency hospital. Its charges are higher than those in the USA. There are a number of locally-registered private medical doctors (general practitioners, or GPs) several clinics and pharmacies. If you as a visitor are vulnerable to any health problem, ask at where you say if they can contact an on-call doctor if needed and bring a plentiful supply of your own medically-prescribed non-narcotic prescriptions.
 Employed
residents must enroll in their employers' insurance-provided healthcare, medical and hospitalization
plans
Employed
residents must enroll in their employers' insurance-provided healthcare, medical and hospitalization
plansAccording to the Health Insurance Act, employers must provide health insurance coverage for all employees working more than 15 hours per week and beyond two months out of the year. Employers must provide the same coverage to an employee’s non-employed spouse. Employers may deduct no more than half of the monthly premium from an employee’s salary or wages towards the enacted health insurance policy. Employees should ensure that they receive health insurance as soon as they start employment, as well as an employment contract outlining their wages and required deductions and itemized pay stubs for their personal records. It is the employee’s responsibility to notify their employer of any changes to their non-employed spouse’s employment status. If an employee seeks medical attention and learns their health insurance policy is not active, they should submit the medical bills to their employer immediately for payment. If an employer is non-compliant with the law and an employee incurs medical bills during a period of non-coverage, under the Act the employer is responsible for paying those medical bills, which are often more expensive than monthly premiums. Employers are encouraged to shop around and purchase a policy that is affordable so that payments can be made on time, thereby avoiding any disruptions in coverage. It is the employer’s responsibility to notify employees if a contract of health insurance is not in effect or if there are any changes to the health insurance policy.
Employers are free to select their own health insurance plan, as long as they comply with certain minimum requirements imposed by the government. Employees are required to accept and sign up for the plans offered by their employers. There is no standard health plan, nor any plans offered by associations which include those employers as members.
All such health plans must be offered by majority-Bermudian owned and operated, not non-Bermudian, companies licensed by the Bermuda Government to provide such services.
Approved Bermudian health/medical private sector insurance companies are
 There is no
standard plan applicable to all employers or employees. An
Employees' share can be 50% of
the employers' private Health Care Insurance Plan often (but not always) including
Major Medical and Dental. If an employee has an unemployed spouse, the
employer concerned must bear part of this cost and may share the cost of
insuring the spouse with the employee. The same cost responsibility and cost
split applies in the case of dependent children of the employee. Working
newcomers to Bermuda are not given a choice by their employers of local healthcare plans
but must accept the plan and its insurer offered by their employer. They will not
be allowed to opt out of the local plan if they belong to any non-local healthcare
plan. Personal partners who are not
spouses are not included as such. Healthcare provisions apply only
to employers and their employees and the latter's family (spouse and children)
when the employee's spouse is not working with another employer. In Bermuda, an
unmarried personal partner or parent or sibling of a Bermudian or non-Bermudian
is not a spouse and has no legal standing or spousal rights or any right to have
health insurance with that other person. Any non-Bermudian personal partner but
not a spouse and all other non-Bermudian visitors including tourists are not
permitted by Bermuda Immigration to stay in Bermuda beyond their specified
vacation or holiday unless there are very special and compelling circumstances
reported in advance to Bermuda Immigration.
There is no
standard plan applicable to all employers or employees. An
Employees' share can be 50% of
the employers' private Health Care Insurance Plan often (but not always) including
Major Medical and Dental. If an employee has an unemployed spouse, the
employer concerned must bear part of this cost and may share the cost of
insuring the spouse with the employee. The same cost responsibility and cost
split applies in the case of dependent children of the employee. Working
newcomers to Bermuda are not given a choice by their employers of local healthcare plans
but must accept the plan and its insurer offered by their employer. They will not
be allowed to opt out of the local plan if they belong to any non-local healthcare
plan. Personal partners who are not
spouses are not included as such. Healthcare provisions apply only
to employers and their employees and the latter's family (spouse and children)
when the employee's spouse is not working with another employer. In Bermuda, an
unmarried personal partner or parent or sibling of a Bermudian or non-Bermudian
is not a spouse and has no legal standing or spousal rights or any right to have
health insurance with that other person. Any non-Bermudian personal partner but
not a spouse and all other non-Bermudian visitors including tourists are not
permitted by Bermuda Immigration to stay in Bermuda beyond their specified
vacation or holiday unless there are very special and compelling circumstances
reported in advance to Bermuda Immigration.
Some expatriate-friendly organizations beyond Bermuda claim to offer their clients from overseas who will be working in Bermuda full hospitalization and medical insurance. But if they are not Bermuda Government approved they should be avoided.
 A recent
Bermuda Government's Adult Wellness Report showed that
A recent
Bermuda Government's Adult Wellness Report showed that
One in three islanders are obese, caused in part by unsatisfactory working conditions - bad air, excessive heat or cold, poor work space, long periods of standing or sitting - cause stress which leads to drink and drug abuse, heart disease and obesity.
12 percent abuse alcohol
The six most frequent health problems are allergies, asthma, migraine headaches, tension headaches, depression and anemia. (But all this is contradicted by reports showing heart attacks and strokes as leading causes of death)
Top health concern is AIDS and sexual diseases, with 52 percent tested for HIV. 55 percent say they receive no education or information from their doctor on sexual practices or family planning.
30 percent of adults use prescription medicines every day
90 percent of women 40 and over have had a mammogram
95 percent of women 40 and over have had a pap smear
60 percent of men 40 and over have had a prostate exam.
Patients who need tests or treatments at bigger facilities beyond Bermuda are first referred by doctors then go by commercial air or air ambulance to hospitals overseas. If patients are not covered by Major Medical insurance when they are referred to an overseas hospital, they have to bear the costs themselves. It will be very expensive. Such services are not provided under HIP in Bermuda. One overseas hospital is the world famous Johns Hopkins Hospital at 600 N. Wolfe Street, Baltimore, Maryland. Its superb, comprehensive Rehabilitation Center is available six to seven hours a DAY including Saturdays. Others include the Lahey Clinic, Massachusetts General, Brigham and Women's, all in MA; and for cardiovascular, the Washington Medical Center in Washington DC.
 Not yet put into effect
but pending:.
Basics were unveiled in February 2011 by the former Government, which aims to
ensure all residents have quality, affordable healthcare. Then-Health Minister
Zane DeSilva said the plan would introduce “wide-ranging and profound”
reforms to the Island’s health care system. It aims to make health care more
affordable and improve access and quality care. Mr DeSilva said the reforms
“address the long-standing concerns with the escalating costs of health care,
and the inequitable burden placed on too many individuals and families. It
pledges to ensure basic and essential care is provided for every Bermuda
resident in 2013. The plan states universal access is “necessary” for the
Island to achieve better health outcomes, such as improving life expectancy and
reducing disparity. Eligibility will be determined on the basis of residence and
will be defined by law. The package of services covered will also be defined in
law. Another goal is to ensure that basic coverage includes urgent physical and
mental health care, hospitalization, primary care, preventative care and
maintenance. It will also include clinical preventative services like screening,
counseling and treatment. The National Health Plan will also ensure health
coverage contributions are based on ability to pay. This will allow health care
costs to be affordable to all members of the community. It also changes the way
health care is defined as treatment will no longer be considered a consumer good
or commodity, but a “public good” that is accessible by need. Currently the
Island compares well with other countries in the Organization for Economic
Cooperation and Development (OECD) in terms of life expectancy, infant mortality
rates and access to health care. But it fares poorly in terms of ensuring all
residents have affordable health insurance coverage which provides a core set of
services. Other goals include ensuring smarter use of overseas care, introducing
an integrated health IT system, health promotion, and re-engineering the way
health care is financed so it can be more cost-effective and ensure better value
for money. When asked how the universal coverage would affect rates people
currently pay, Mr DeSilva said: “Those who can pay will pay, and now those
that are struggling to pay, we want to make sure they don’t pay or pay very
little. The system we have right now is very unfair.”
Not yet put into effect
but pending:.
Basics were unveiled in February 2011 by the former Government, which aims to
ensure all residents have quality, affordable healthcare. Then-Health Minister
Zane DeSilva said the plan would introduce “wide-ranging and profound”
reforms to the Island’s health care system. It aims to make health care more
affordable and improve access and quality care. Mr DeSilva said the reforms
“address the long-standing concerns with the escalating costs of health care,
and the inequitable burden placed on too many individuals and families. It
pledges to ensure basic and essential care is provided for every Bermuda
resident in 2013. The plan states universal access is “necessary” for the
Island to achieve better health outcomes, such as improving life expectancy and
reducing disparity. Eligibility will be determined on the basis of residence and
will be defined by law. The package of services covered will also be defined in
law. Another goal is to ensure that basic coverage includes urgent physical and
mental health care, hospitalization, primary care, preventative care and
maintenance. It will also include clinical preventative services like screening,
counseling and treatment. The National Health Plan will also ensure health
coverage contributions are based on ability to pay. This will allow health care
costs to be affordable to all members of the community. It also changes the way
health care is defined as treatment will no longer be considered a consumer good
or commodity, but a “public good” that is accessible by need. Currently the
Island compares well with other countries in the Organization for Economic
Cooperation and Development (OECD) in terms of life expectancy, infant mortality
rates and access to health care. But it fares poorly in terms of ensuring all
residents have affordable health insurance coverage which provides a core set of
services. Other goals include ensuring smarter use of overseas care, introducing
an integrated health IT system, health promotion, and re-engineering the way
health care is financed so it can be more cost-effective and ensure better value
for money. When asked how the universal coverage would affect rates people
currently pay, Mr DeSilva said: “Those who can pay will pay, and now those
that are struggling to pay, we want to make sure they don’t pay or pay very
little. The system we have right now is very unfair.”
The plan sets out 11 health sector goals to improve access, quality and
efficiency, which will be implemented over the next two to six years, with
specific goals.
Spouses of the opposite sex (not personal partners who are not legally recognized as such and have no legal rights in Bermuda) of incoming non-Bermudian working newcomers who are non-Bermudian and not working must be covered for health insurance by the other spouse's employer.
2020. March 23. Twenty ventilators are available at the island’s general hospital and eight more are on their way, the Bermuda Hospitals Board said last night. A BHB spokeswoman added there was also a plan to look after critical patients outside King Edward VII Memorial Hospital’s intensive care unit if the Covid-19 pandemic caused widespread serious illness. She said: “This is an exceptional situation. There is not a hospital or healthcare system that is built, supplied and staffed to be ready for a pandemic like this.” The spokeswoman added the board had still to get an estimated time of arrival for the extra ventilators. However, she said the equipment — machines that help patients with respiratory problems to breathe — was only part of the equation. She explained: “You need bed spaces where there is oxygen available, and critical care staff who are specially trained to look after ventilated patients. Although Covid-19 most significantly affects the lungs, all critically ill patients are at risk of multiple organ failure, so this specialized critical care training is vital. So our ability to care for critically ill Covid-19 patients relies equally on equipment, such as ventilators, staff and space. For this reason, we are looking at increasing our capacity outside of the intensive care unit at KEMH and utilizing all bed space with available oxygen.” The spokeswoman said increasing acute and critical care bed capacity was an immediate priority, as well as “cross-training and upskilling” existing staff. KEMH suspended elective surgeries last week to start the training. The hospitals board will also collaborate with “healthcare colleagues in the community” for extra back-up. KEMH has 120 acute care beds, with 90 in the acute care wing and 30 in the general wing. There are nine beds in the ICU. The acute care beds were 80 per cent occupied and the ICU beds were 77 per cent occupied last Friday evening. The bed occupancy varies and is monitored daily. The BHB spokeswoman said: “Our current plan is to use other areas of the hospital for ventilated patients. Today, we could care for up to 20 people on ventilators. When our additional ventilators arrive, we will be able to use them all.” She added: “We are working with Government to discharge at least 30 long-term care patients, use operating room spaces and other ward areas. Some good news is that we were in the middle of a bed replacement programme.” The spokeswoman said 48 new beds would arrive today and would be used immediately if needed. BHB had 420 nurses — 383 full time and 34 casuals — 118 doctors, 203 nurse aides (165 full-time, 37 casuals, one temporary) on staff in February. There were also 31 emergency medical technicians — 22 full time, eight casuals and one part-time. The spokeswoman said: “There are additional nurses in administrative and leadership functions and nurses and doctors in the community who can also add to these numbers in a time of crisis, especially if staff themselves are ill or in quarantine.” About 40 of BHB’s nurses have critical care training, along with 12 anesthetists, plus two doctors outside the hospital with training who could support, and 13 emergency department doctors. The spokeswoman added: “There are also certain speciality doctors and nurses in the hospital and community who can help work to support Emergency Department and inpatient care. This will need to be a team effort to get through.” A study by the Harvard Global Health Institute released last week warned that US hospitals could be overwhelmed by the illness. The review suggested that in a worst-case scenario, 60 per cent of the US population would get Covid-19, with a moderate scenario of 40 per cent and a best-case scenario of 20 per cent. Those numbers were specific to the US. The study predicted 20 per cent of adults who caught the coronavirus would need hospitalization and 20 per cent of those hospitalized would need a ventilator. Premier David Burt said last night that although there were six confirmed cases in Bermuda, there had not yet been one that required hospitalization. He said in a Facebook Q&A on Saturday that the Government had imposed strict measures to limit community spread of the virus here. The Premier added: “I do not have a concern that our hospital will be overrun and I have no intention of letting us get to that particular point at all.” Bermuda’s population was 63,779, with 17 per cent aged over 65, in 2016, according to the census. The BHB spokeswoman said: “It is sobering looking at numbers and our hope is that people pay attention as they are the front line of protection and can help us towards the best case scenario, which would be most manageable. As healthcare workers on the frontline, we will do everything we can. The healthcare community is pulling together, and we are planning, testing and looking into every option we have to cope.” She added: “This is why we cannot stress strongly enough that the community actions now — social, physical distancing; washing hands; not touching our eyes, nose and mouth; adhering to quarantine and isolation guidelines; and staying at home — are the most important actions that will enable the healthcare system to cope, along with on-island testing, and border control. This gives us the chance to slow and maybe even eradicate the virus in Bermuda.”
Covid-19 statistics
2020. March 21. The health system could be “overwhelmed” if the public fails to follow quarantine and isolation rules, the Bermuda Hospitals Board’s chief of staff warned today. Michael Richmond said that the BHB backed “decisive action” by the Government to limit the spread of Covid-19. However, he added: “The community must adhere to these restrictions, abide by quarantine and isolation rules, or else the healthcare system could be overwhelmed as has happened in countries such as Italy. The BHB is doing everything in its power to prepare for increased demand. But we have limits. If we as a community do not control the spread of Covid-19, the numbers of critically ill patients could rise precipitously and the ability for the healthcare system to support those who are most critically ill will be put at risk.” The warning came as the BHB announced further restrictions at its hospitals and departments. A spokeswoman for the BHB said that people who had to visit the Emergency Department should come by themselves, if possible, and should bring only a single companion “if essential. This is to reduce the number of people in the waiting room, and help emergency patients, who are more likely to be in an at-risk group, to maintain a physical distance from each other while they wait. Parents who are seeking treatment for themselves are advised not to bring their children with them.” The spokeswoman said that people should not visit patients other that in “exceptional circumstances, such as newborns — the mother’s partner or one close relative or friend if there is no partner — unwell children — parents only, or people near the end of life”. She added that other outpatient services were being “critically reviewed with the aim of only seeing people in person by exception. All other patients will either have appointments postponed if they are stable, or offered a remote consultation, for example, by phone. People with outpatient appointments will be contacted directly about what will happen.” She added that elective hyperbaric treatments, used for divers with the bends and sometimes for wound care, had been suspended and that BHB was looking at closing down the service “even to emergency treatments. These are mostly diving accidents, but the oxygen from the hyperbaric chamber will be needed if multiple people with Covid-19 need ventilator and/or oxygen support in the hospital.” Diagnostic and lab tests are by appointment only and urgent tests had been prioritized over routine ones. Dr Richmond said that the measures were designed to limit opportunities for Covid-19 to spread by a reduction in foot traffic and a cut in the number of people in waiting rooms. He added: “This supports physical distancing that, along with hand washing and not touching your eyes, nose or mouth, are key ways people can protect themselves and their families.”
2020. March 18. New restrictions on blood donations have been put in place because of the coronavirus pandemic — but new donors are still needed. The Bermuda Hospitals Board said people cannot donate blood if they have either been to an area with an outbreak of Covid-19 in the past 28 days or lived with someone diagnosed with, or suspected of being infected with Covid-19 over the same period. Anyone with a confirmed case of Covid-19 will be banned from blood donation until 56 days after they have made a full recovery. A Bermuda Hospitals Board spokeswoman said: “Our screening measures are evolving in line with public health recommendations and the changing dynamics of the Covid-19 outbreak. We ask donors who have recently travelled outside of Bermuda to call 236-5067 when booking their appointment to confirm they are eligible. These measures help ensure our donor centre remains an area of wellness within Bermuda’s health system — the Blood Donor Centre is not a place where sick people gather. We urge all healthy eligible donors to book and keep appointments. Patients depend on these life-saving donations. Every day, blood products are needed for patients undergoing surgery, cancer treatments and to save lives following traumas. To help every patient, we require the ongoing generosity and commitment of donors.” The spokeswoman said it was safe to donate blood in Bermuda and all donors were screened for any symptoms of illness. She added: “This screening occurs during both appointment booking and upon arrival at the donor centre. Those with any symptoms are not allowed to donate blood and are instructed not to visit.”
2020. March 10. The country must come together “like never before” as Bermuda braces itself for the battle against a new and killer strain of coronavirus, the health minister said yesterday. Kim Wilson said the kind of co-operation shown in hurricanes was needed and that people had to work together to limit the spread of Covid-19, although she emphasised the island had no confirmed cases. She told MPs in a presentation on the Ministry of Health’s budget for 2020-21: “I will take this time to remind us all that we are in the phase of preparedness for a potential pandemic and we must focus on preparing for this situation. The World Health Organisation says we must prepare to detect cases, prepare to treat cases, prepare to follow contact and prepare to put in place adequate containment measures to control the spread.” Ms Wilson added: “If I could, I would stand here today and use the entire five hours allocated to this ministry and appeal to all, how such an historic threat can only be managed by the highest level of collaboration and solidarity, of every single sector and person, in this community. This community has proven to be resilient against catastrophic hurricanes when we band together as one, so I also ask that we rise to the occasion for this unexpected and unusual threat to health like we have never done so before.” Ms Wilson said that her ministry had been preoccupied by the respiratory disease since mid-January. She added that her team was “aggressively, progressively and very passionately preparing for the escalating health threat. We’re working closely with our many international affiliates, other ministries, departments, the hospitals, the community providers and other agencies to expeditiously investigate and monitor the activities. Depending on the extent of which the Covid-19 threat evolves, the ministry may be engrossed in work completely dedicated to managing the situation during fiscal year 2020-21.” Ms Wilson added that the entire workforce in the Chief Medical Officer’s department was “nearly fully dedicated to the planning and preparing for Covid-19, which is rapidly spreading across the globe. It is a highly infectious disease and a rapidly escalating threat. Therefore it is a threat to Bermuda now and in the foreseeable future. There have been no cases of Covid-19 identified in Bermuda — however, the reality is that the spread of the virus continues on track to become a pandemic in the coming weeks if not days. Although Covid-19 is not in Bermuda, it has been documented in over 109,000 people in over 100 countries, including our region.” Ms Wilson said that the Bermuda Hospitals Board had an emergency plan in place that included options for its emergency, intensive care unit and acute care wards “to cope with an influx of patients in the event of a pandemic. The availability of beds can change on a daily basis. However, BHB has taken actions to increase the capacity of availability by making adjustments such as discharging stable patients, postponing elective surgeries and using additional beds in other areas. There are negative pressure rooms in emergency and on each floor of the acute care wing. Negative pressure rooms stop the air flowing out of the patient’s room, keeping the rest of the hospital safe. There is also an entire floor, inclusive of 30 beds, with an independent air filtration system should that need arise in case it needs to be used for potential cases. It would be critical for people who can be cared for at home to stay there so that hospital services can focus on those most in need.” She said that no one should arrive at the hospital or any clinic without calling first to tell staff their symptoms and get advice on what to do next. Scott Pearman, a One Bermuda Alliance MP, asked what happens to homeless people if there was an outbreak as they would be unable to “self quarantine” at home. He said: “It seems like a quite sensible question in the circumstances.” Ms Wilson responded that the Government is in the process of identifying facilities for those who may be in that position.
2020. March 7. The Bermuda Hospitals Board will complete its annual reports up to 2019 by the end of this year, health minister Kim Wilson told MPs yesterday. Ms Wilson announced BHB’s financial statements for 2015 and 2016 had unqualified audits as she tabled the quango’s annual report for 2015 in the House of Assembly. She added: “The focus is now on completing the audits for 2017, 2018, 2019 and finally 2020. The current anticipated schedule will see BHB completing all its audits up to 2019 by the end of the calendar year.” The BHB came under fire last month after it was five years behind with its audited accounts. Auditor-General Heather Thomas said that 29 public authorities, including the BHB, were so far behind with their books that politicians and officials could not make effective decisions on how to spend public money. Ms Wilson said: “I look forward to bringing the future annual reports as they are made ready and to see BHB move forward on its legislated schedule of financial reporting.” The minister added 2015 was an “incredible year” as BHB moved acute services into the new acute care wing after years of construction. She said: “BHB was able to meet its new financial obligations even though revenue decreased that year. Significant cost controls were put in place and discretionary spending was carefully managed.”
2020. March 6. Problems with two out of three industrial washing machines has cut the Bermuda Hospitals Board’s laundry capacity, as the island braces itself for the possible impact of a potential killer coronavirus. However, a spokeswoman for BHB said a back-up plan had “ensured that there has been no impact to services at BHB” as outside laundries had been pressed into service. She added: “Our mitigation strategy also covers dealing with surges. This has to be planned for, as surges can happen at any time, due to flu or major incidents, event without the new coronavirus.” The spokeswoman said the BHB laundry department had four heavy-duty washing machines, but that one had not been in use for “many years”. She added that the three operational machines had all suffered breakdowns. The spokeswoman said: “Two of the machines went down this week, and one in mid-February. One of them has been repaired with parts fabricated by a local machinist and is already back in operation. The two other machines require overseas parts which have been ordered, and the parts are expected next week.” The spokeswoman said that BHB was able to meet demand with “at least two, and certainly with three, machines”. She added: “If the overseas parts arrive as expected, we should be able to fully support our internal needs by the end of next week.” The information was released after questions sent to the BHB by The Royal Gazette yesterday. The spokeswoman said that the laundry department was used by the King Edward VII Memorial Hospital, the Mid-Atlantic Wellness Institute in Devonshire, as well as group homes. She added: “Because it is a critical support service, we have mitigation and emergency plans in the event of a critical failure and this plan has been activated. This includes outsourcing work to a local company, who is able to help until we are back to full capacity. The immediate activation of our plan has ensured that there has been no impact to services at BHB.” The spokeswoman said that in the long term the BHB had planned “a more extensive laundry upgrade with new equipment”. She added: “This is currently going through internal approval processes.”
2020. February 20. Cuts could be made to the price of prescription drugs if the Government worked with other countries to negotiate better rates, the health watchdog’s chief executive said yesterday. Dr. Ricky Brathwaite, head of the Bermuda Health Council, explained that the organisation was looking at how to save money on drug procurement. Dr Brathwaite said: “The global market is pretty volatile when it comes to prescription drugs, especially if you don’t have leverage. One of the things that the Pan American Health Organisation always says is that countries by themselves will never get the best prices for drugs … they say the best way to get good prices for drugs, is to partner with other countries and purchase with them. Not only do we not partner with other countries in purchasing, but even within Bermuda, we have individual pharmacies purchasing, or we have a small pharmacy group purchasing, or we have BGA. So we’re never going to get, from a volume standpoint, the best prices for drugs unless we do it cooperatively.” Dr Brathwaite added that raised the question of whether the Government needed to “step in to help in the procurement process to negotiate from a country to country standpoint, instead of a private business to country standpoint. It doesn’t happen currently, but it’s something that we do recommend — that the Government does get a little more involved in the procurement of drugs. People may say it’s ‘more government involvement’, but the reality is that a government ... is always going to get more leeway in terms of negotiation than a private business, especially when it comes to these kinds of big things. For example, in the eastern Caribbean there must be eight, nine or ten countries that work together in purchasing and they’ve achieved 20 per cent savings in their drugs.” Dr Brathwaite said that Bermuda was “totally dependent on the global market for drugs”. He explained that unless there were strong relationships or negotiating arrangements with pharmaceutical companies, buyers were prone to price hikes. Dr Brathwaite said: “The Pan American Health Organisation (PAHO) does bulk purchasing for multiple countries, on some drugs. There is huge benefit to co-operative procurement. We haven’t even touched the surface of our ability to effect and impact our drug prices, in a positive way, by doing that. We’re spending a lot of money on prescription drugs and we’re expecting to spend a lot more money on prescription drugs, not only as the market for prescription drugs becomes more modern and they offer more drugs for more things, but as our population ages. Since we haven’t started in the best place when it comes to chronic disease and it takes a while for a population to get healthier, we anticipate that the need for prescription drugs is going to increase.” The Paho explained on its website that its Strategic Fund was set up in 2000 “to facilitate the acquisition of strategic public health supplies” for its member states. The website added: “Through technical support in procurement, the fund promotes the continuous availability of quality strategic supplies at low cost.” It highlighted that 33 countries in Latin America and the Caribbean had signed agreements with Paho by June 2018 to use the fund. Bermuda was included on its list. Dr Brathwaite said that education was needed to make people aware of the importance of taking medication as prescribed. "When you don’t take your drugs, even if you miss a day, the outcome that the drug is supposed to provide gets impacted and that leads to all kinds of other complications.” The health economics expert added: “We have to get people healthier in general so that they don’t need prescription drugs in the first place.” He said that drugs procurement was among several areas of law that the health council hoped to see updated in the coming year. Other areas included regulations about what information must be included in health insurance claims and legislation that related to artificial limbs. Mark Selley, the Bermuda Healthcare Advocacy Group chairman, said he heard about proposals for the island to work collaboratively in the procurement of prescription drugs about two years ago from the former BHeC chief executive Tawanna Wedderburn. He added: “I support it 100 per cent, I just need them to get on with it. It would be a huge advantage to patients. Everybody will save. People like me who need medication for life — it’s a huge benefit in saving. So many are taking shortcuts with their meds to save, instead of taking every day, they’re taking every other day and trying to stretch them out, not understanding the full ramifications of what that means.” The then One Bermuda Alliance administration’s 2015 Throne Speech said that the Government would run a pilot programme to increase access to key drugs, in efforts to help people who could not afford the medication they need to treat chronic conditions. The Throne Speech said: “The programme is based on joining the Pan American Health Organisation’s Strategic Fund to procure selected drugs for Government programmes at favourable rates.” A spokeswoman for the Ministry of Health said that the ministry had joined the fund, which was used by the Bermuda Hospitals Board to obtain medicines. She added: “The Minister of Health is conscious of the difficulties many people in our community are having, as it relates to the high cost of healthcare, and the purchase of prescription drugs is one part of that high expense. For this reason, the health council is working on initiatives to make medications more affordable, with the ministry’s full support.”
2020. February 19. The Bermuda Hospitals Board has made public its unaudited financial information for the past three years, revealing that its annual salary bill has risen to almost $200 million. A statement from the board said that between 2017 and 2019, salaries and benefits, including overtime and casual staff costs, as well as regular salaries, rose 3 per cent from $188.7 million to $194.3 million. The statement said: “Comparing the three full fiscal years between 2017 and 2019, total revenue rose from $324.7 million to $329.8 million between fiscal year 2017 and 2019, a rise of $5.1 million or 1.5 per cent over three years. The dip in revenue for 2018 represents a one-off $25 million cut in hospital subsidy. Total expenses rose from $316.8 million to $329 million over this time period, representing $13 million or 3.9 per cent in total. A substantial increase was experienced in repairs and maintenance, which increased from $18.9 million to $26.9 million, which is 42 per cent or $8 million. This reflects the increasing cost of keeping the ageing King Edward VII Memorial Hospital general wing and Mid-Atlantic Wellness Institute facilities safe for patient care.” The statement added: “In the fiscal years 2017 to 2019, BHB revenue was substantially made up of fee-for-service charges, with the addition of a MWI grant and a partial grant for long-term care. In June 2019, BHB moved to a fixed government grant of $322 million.” The board was criticized last week in Parliament by independent senator James Jardine for failing to release audited financial statements to the public for the past five years. Auditor-General Heather Thomas told The Royal Gazette that the quango was one of 29 publicly funded bodies whose financial statements were in arrears. Yesterday’s statement from the hospitals board said: “BHB is releasing internal management accounts data from fiscal year 2017, up to and including the third quarter of fiscal year 2019, the latest quarter available. These represent the data shared with staff and the board, but are unaudited. BHB will continue to provide internal management accounts data quarterly and update information online, as BHB does with its quarterly posting of quality patient safety data, annual plan of projects, statistics by fiscal year, and patient satisfaction data by fiscal year.” She said the board’s website provided further statistics, details of projects and strategy documents. The spokeswoman noted that the BHB published a clinical services plan in 2018 to “address improving the health and care of Bermuda’s community, with better community management of chronic illness, and a stronger safety net after discharge, to reduce the need for expensive hospital services”. She said it had also developed a financial recovery plan to manage the $25 million cut in hospital subsidy in the financial year 2017-18. The board is pursuing legal action to keep the six-figure salaries of its top executives a secret after the Information Commissioner ordered it to disclose the total cost of each position, within $10,000 bands.
2020. February 18. Three health insurers have confirmed that they had no involvement with Patients 1st movement. They were responding to claims by David Burt, the Premier, that insurers were running the group. Patients 1st has raised concerns over the impact of government healthcare financing reforms. In the House of Assembly last Friday, Mr Burt took a swipe at Patients 1st, saying: “How is it possible that we have had an organisation that has existed for three months and nobody knows who is running it?” He added: “It’s being run by the insurance companies. And they are not going to show their faces, because they are trying to protect their profits.” Patients 1st described Mr Burt’s statement as “absolutely untrue” and added that it had never received funding from any insurer, nor had there been any involvement from any insurance company representatives. The Royal Gazette reached out to health insurers for comment. John Wight, chairman and chief executive officer of BF&M, responded: “As is indicated in the Patients 1st statement, BF&M denies any involvement with Patients 1st. However, much like Patients 1st, we are acutely concerned about the potential impact of healthcare funding reform for our customers and the broader community. In that regard, we are proud of the fact that we took an industry lead to educate our policyholders about such a complex and critical issue. We will continue to engage with the Government and with our customers, providing valuable input to the discussion.” A spokesperson for Argus said: “As Bermuda’s healthcare environment evolves, Argus remains committed to helping to drive down health costs while maintaining access to quality care through working with the Government and other stakeholders. However, Argus has no involvement with Patients 1st.” Naz Farrow, the CEO of Colonial Group International, said: “Like many people in the community, we are extremely concerned about the possible impact of Government’s health care reform on the community, however it is wrong to suggest that we are involved in running Patients 1st. She added: “We continue to be happy to engage with the Government over their proposals.” A meeting held by Patients 1st in Queen Elizabeth II Park on February 7 attracted hundreds of people, who heard speakers express concerns that the Government’s plans would limit healthcare choices for patients. Since then, government backbencher Jason Hayward, as well as Mr Burt, have each attacked the group, labeling it “Profits First”.
2020. February 18. A review team to assess proposals for tackling chronic disease in Bermuda is being sought by the Bermuda Health Council. The BHeC announced last year that $2 million was available to fund brainstorming on tackling Bermuda’s high costs of non-communicable chronic disease, such as diabetes, high blood pressure and heart disease. The maximum awarded for ideas submitted is $200,000. The first round of suggestions has been approved, according to the council’s chief executive, Ricky Brathwaite. Prospective members of the review panel will be required to work with a team and hold relevant knowledge or qualifications. A council statement said suggestions would be considered on a “continuous basis”. But the Chronic Disease Innovation Programme is also being held to a timeline. For more information on the Chronic Disease Innovation Programme, call 292-6420.
2020. February 17. Premier David Burt has challenged the pressure group Patients 1st to reveal its identity and meet with him over its campaign against proposed changes to the health insurance system. Speaking in the motion to adjourn in the House of Assembly on Friday, the Premier called the group “Profits First”. He told MPs: “How is it possible, that we have had an organisation that has existed for three months, and nobody knows who is running it?” Mr Burt added: “It’s being run by the insurance companies. And they are not going to show their faces, because they are trying to protect their profits.” In a response yesterday, the group called the statement “absolutely untrue”, and said it had “never received funding from any insurance company”. Nor was there any involvement by insurance company representatives, although the statement said it would “welcome them into our discussions”. Patients 1st added: “We wish to come together with the insurance companies and Government, to arrive at real solutions to improve delivery of healthcare to the underinsured and uninsured, without reducing the quality of care and broad cover that the population of Bermuda has come to expect.” In his remarks on Friday night, Mr Burt threw down the gauntlet to the group, challenging its leaders to “come to my office” this week. “Tell me when you want to come,” Mr Burt said in the House. “Let’s sit down and have a talk. Show your face.” Mr Burt said that Kim Wilson, the Minister of Health, had reported being contacted by the group in an e-mail asking to meet at the end of March. He added: “Bring it. Let’s have that chat.” Patients 1st acknowledged it had “privately and purposely invited consultation with the Minister of Health last week as noted by the Premier for a meeting in March”. The statement yesterday added: “The purpose of which is to work together on solutions with a representative present from every healthcare dimension — something that the medical community has asked Government for on numerous occasions, and to date have been refused.” The group came forward last November in opposition to the Government’s draft Bermuda Health Plan 2020. Patients 1st said yesterday it was a collaboration, without leaders, of more than 12,000 “concerned patients, community groups, private citizens, physicians, pharmacists, dentists, chiropractic doctors and allied healthcare workers encompassing all socioeconomic groups”.
 2020.
February 8. Hundreds of people gathered in a Hamilton city park yesterday in a
protest over a controversial plan to overhaul the health insurance system.
Speakers at the event, organised by campaign group Patients 1st, said efforts
should be made to improve the existing healthcare system rather than a major
change. Ronda James, a dentist, said she had backed healthcare reform, but felt
“bullied” into a healthcare system that focused more on money than its
patients. Dr James added: “All we are getting from the Ministry of Health
these days is a push for a single-payer scheme. I’m disappointed. The ministry
started a conversation that had the potential of making real and positive change
for the health of Bermuda. Instead, that conversation has been pushed aside for
a scheme that not only doesn’t help to make us healthier, but also takes away
our choices and carries the potential of limiting access to healthcare that
people may need. These people don’t treat patients, don’t provide patient
care and they don’t see a patient suffer. Doctors are prepared to work with
the Government to improve healthcare, but that the medical profession appeared
to have been ignored. I don’t see how changing my insurance policy is going to
improve healthcare. In fact, I see a greater likelihood of it doing the exact
opposite.” Dr James was speaking after the event, held at Queen Elizabeth II
Park on Queen Street. Janie Brown, also a dentist, said a unified health plan is
not the same as a universal healthcare plan and that it will not help the 10 per
cent of the population that had no health coverage. She said: “Most of our
citizens would have a healthcare plan — I can’t say all because the same 10
per cent would likely not be able to afford the unified plan any more than they
can afford HIP.” Dr Brown added that under a unified health plan the
Government would control the cost of premiums and the services provided. She
said: “Most unified healthcare plans have preventive care and emergency care,
nothing more. All other procedures are paid out of pocket by patients, or
through expensive supplemental insurance. This type of system requires large
sums of money to fund to success, which means heavy taxation. We believe we can
achieve universal healthcare without dismantling the present system, which
works. We want to just make changes to make it better.” Burton Butterfield, a
GP, said: “Bermuda does not need to make wholesale changes to a system that
has been working so well. Right now, most of us have access to the best of care,
we have access to secondary and tertiary care at some of the best institutions
in the world. Government has been making changes without involving the
stakeholders.” Dr Butterfield added that up to 45 per cent of the island’s
healthcare costs were linked to the cost of the acute care wing of the King
Edward VII Memorial Hospital. He said: “The major issue we have, at this
particular time, are the few people who have either no insurance or not enough
insurance. Maybe that’s all that needs to be addressed, at this point in time,
instead of wholesale changes to the whole system.” A spokeswoman for the
health ministry said the Government was pleased by the broad support for its
proposals. She added: “This shows that the organisation shares the
Government’s goal to ensure everyone in Bermuda can access the healthcare that
they need. It was encouraging to see a large turnout at the event, as healthcare
is a topic which affects everyone, and change in this sphere is something which
does, and should involve, all of us. This Government is committed to achieving
access to healthcare for all and bringing down the costs of healthcare in
Bermuda, which are unsustainable.” Kim Wilson, the Minister of Health, added a
speech by Martha Dismont, the executive director of Family Centre and the final
speaker at the event, struck a chord with her. Ms Wilson said: “She
highlighted the need to work through differences together. I welcome the
opportunity to have dialogue, real, actual, meaningful dialogue, with Patients
1st, on our shared goal for universal healthcare. I believe we have more in
common than differences and, as Mrs Dismont said, we will find the best
solutions together.”
2020.
February 8. Hundreds of people gathered in a Hamilton city park yesterday in a
protest over a controversial plan to overhaul the health insurance system.
Speakers at the event, organised by campaign group Patients 1st, said efforts
should be made to improve the existing healthcare system rather than a major
change. Ronda James, a dentist, said she had backed healthcare reform, but felt
“bullied” into a healthcare system that focused more on money than its
patients. Dr James added: “All we are getting from the Ministry of Health
these days is a push for a single-payer scheme. I’m disappointed. The ministry
started a conversation that had the potential of making real and positive change
for the health of Bermuda. Instead, that conversation has been pushed aside for
a scheme that not only doesn’t help to make us healthier, but also takes away
our choices and carries the potential of limiting access to healthcare that
people may need. These people don’t treat patients, don’t provide patient
care and they don’t see a patient suffer. Doctors are prepared to work with
the Government to improve healthcare, but that the medical profession appeared
to have been ignored. I don’t see how changing my insurance policy is going to
improve healthcare. In fact, I see a greater likelihood of it doing the exact
opposite.” Dr James was speaking after the event, held at Queen Elizabeth II
Park on Queen Street. Janie Brown, also a dentist, said a unified health plan is
not the same as a universal healthcare plan and that it will not help the 10 per
cent of the population that had no health coverage. She said: “Most of our
citizens would have a healthcare plan — I can’t say all because the same 10
per cent would likely not be able to afford the unified plan any more than they
can afford HIP.” Dr Brown added that under a unified health plan the
Government would control the cost of premiums and the services provided. She
said: “Most unified healthcare plans have preventive care and emergency care,
nothing more. All other procedures are paid out of pocket by patients, or
through expensive supplemental insurance. This type of system requires large
sums of money to fund to success, which means heavy taxation. We believe we can
achieve universal healthcare without dismantling the present system, which
works. We want to just make changes to make it better.” Burton Butterfield, a
GP, said: “Bermuda does not need to make wholesale changes to a system that
has been working so well. Right now, most of us have access to the best of care,
we have access to secondary and tertiary care at some of the best institutions
in the world. Government has been making changes without involving the
stakeholders.” Dr Butterfield added that up to 45 per cent of the island’s
healthcare costs were linked to the cost of the acute care wing of the King
Edward VII Memorial Hospital. He said: “The major issue we have, at this
particular time, are the few people who have either no insurance or not enough
insurance. Maybe that’s all that needs to be addressed, at this point in time,
instead of wholesale changes to the whole system.” A spokeswoman for the
health ministry said the Government was pleased by the broad support for its
proposals. She added: “This shows that the organisation shares the
Government’s goal to ensure everyone in Bermuda can access the healthcare that
they need. It was encouraging to see a large turnout at the event, as healthcare
is a topic which affects everyone, and change in this sphere is something which
does, and should involve, all of us. This Government is committed to achieving
access to healthcare for all and bringing down the costs of healthcare in
Bermuda, which are unsustainable.” Kim Wilson, the Minister of Health, added a
speech by Martha Dismont, the executive director of Family Centre and the final
speaker at the event, struck a chord with her. Ms Wilson said: “She
highlighted the need to work through differences together. I welcome the
opportunity to have dialogue, real, actual, meaningful dialogue, with Patients
1st, on our shared goal for universal healthcare. I believe we have more in
common than differences and, as Mrs Dismont said, we will find the best
solutions together.”
2020. February 5. Patients 1st Bermuda, a pressure group with 10,000 supporters to improve healthcare reform, is hosting a ‘Health Plan Talk in the Park’ this Friday Feb 7th. The group was started by concerned medical professionals and has now grown to a community force of patients, pharmacy owners, dentists, chiropractors, community leaders, business owners, charities and natural healers. Patients 1st Bermuda is now a community group working to ensure that the health needs of the already vulnerable are not further at risk from the unforeseen consequences of health reform financing, as set out in Bermuda Health Plan 2020. The movement has attracted people from all parts of the community beyond health care because of a community concern that Bermuda is at a crossroads on many volatile issues. In addition to healthcare, the community is concerned about immigration policy, energy regulation, international business, gaming, tourism, education, and criminal justice. A Patient’s 1st organizer said; “With faith in each other and love in our hearts, we must now create an approach to healthcare reform that protects the vulnerable without reducing the quality of care. Friday’s lunchtime event is open to all, regardless of your view about healthcare reform. The Talk in the Park is a way for people to be heard and to learn more about what health reform means to them. Everyone seems to have questions and this is an opportunity to share solutions. This event will pay tribute to our 10,000 supporters by putting patients first, not politics.” The public is invited to bring their lunch to listen, share and learn at Par-la-Ville Park, Queen Street (now named Queen Elizabeth Park) - next to the Bermuda National Library - at 12.30pm to help shape the future of the Bermuda Health Plan 2020 for good. Speakers for the lunchtime event include community leaders, natural healers, performing artists and medical practitioners.
2020. February 1. The acting chief executive of the Bermuda Health Council has been appointed to the role on a permanent basis. Dr Ricky Brathwaite, who has held the top job at BHeC since the controversial dismissal of Tamara Wedderburn in December 2018, was confirmed in the position on January 14. He said: “It is important that we keep pushing for improvements in every part of our health system. There are a lot of headwinds to combat related to population ageing, chronic disease and the global economy. The role of the health council is to provide expert strategy, programmes and advice on guiding the health system through these winds.” Dr Brathwaite, who has more than 15 years’ experience in healthcare and biomedical research, joined the health council as the programme manager of health economics in 2014 and later became the director of health economics. He oversaw the health council’s management and operations in his stint as acting CEO. The health council said the CEO position had a salary of between $168,652 and $219,289 and that Dr Brathwaite was chosen after a “three-month comprehensive search and interview process”. The council added that he had led an international effort to develop solutions to help hospitals and medical practices in their delivery of life-saving care. Dr Brathwaite said: “While there are very specific goals that we have for regulating, co-ordinating and enhancing the delivery of health services here, we also have a great opportunity to be an international example and training ground for Bermudians to become leaders on health system issues globally. I am excited to continue this journey, and hope that the amazing work that our board and secretariat do will positively impact each member of our 64,000-person community.” Dr Brathwaite said the health council would be searching for other Bermudian candidates for other positions within the council.
2020. January 29. People were warned to avoid the hospital’s emergency room unless it was a genuine health crisis as the island prepared itself for potential cases of a killer virus. Michael Ashton, the Bermuda Hospitals Board chief of medicine and infectious diseases specialist, said the plea to keep away from the King Edward VII Memorial Hospital’s emergency room was issued because of the threat from a new strain of coronavirus from China that has killed more than 100 people and has spread to 16 countries. Dr Ashton added: “We are closely monitoring this novel coronavirus and continue to work closely with Government. “BHB has detailed plans for dealing with outbreaks and epidemics and we swiftly reviewed our admissions processes as a precaution. We would ask that people only come to the hospital emergency department if they truly have an emergency situation.” Dr Ashton told the public: “If you are concerned that you may be infected, please call your family doctor or the emergency department before you arrive, as people in the same waiting area could be otherwise put at risk.” The death toll for the killer bug was reported as 106 yesterday and the number of confirmed infections doubled in a day to more than 4,500. The first case in Europe from human-to-human transmission of the virus was found in Germany. The Ministry of Health said on Monday it had raised the threat level from the coronavirus from “guarded” to “elevated” and its epidemiology and surveillance unit was in a “state of heightened preparedness for a public health emergency”. A ministry spokeswoman said yesterday that people who had travelled to areas that placed them “at some risk” from the virus, known as 2019-nCoV, would be assessed using World Health Organisation standards of care for patients with suspected coronavirus. She added: “The Ministry of Health will not make public comments on these instances, however, when a situation arises that is a matter of public safety, information will be shared.” A Bermuda Hospitals Board spokeswoman said: “BHB can confirm that even though the current threat to Bermuda residents is low, we are closely monitoring developments and are ready to respond should the threat increase. BHB has questions in its admission process that identifies anyone who has travelled to a place where there have been known infections and we are ensuring we have all necessary supplies. BHB has protocols in place as part of day-to-day running of the hospitals to minimise the spread of infectious diseases. Measures include negative pressure rooms in the emergency and the acute care wing units that are checked daily and infection prevention protocols such as using protective equipment and clothing. We also have plans in place that enable us to deal with outbreaks and epidemics that could be triggered if the mode of transmission changes and global infection rates continue to increase.”
2020. January 28. Bermuda braced itself yesterday for a potential public health emergency over a killer virus. The Ministry of Health said it had raised the threat level from the coronavirus from “guarded” to “elevated” and that its epidemiology and surveillance unit (ESU) was in a “state of heightened preparedness for a public health emergency”. Kim Wilson, the health minister, said: “Bermuda’s routine public health surveillance activities have been increased, through the well-established collaborations between the ESU and the hospital, physician’s offices and customs and immigration departments.” Ms Wilson said “enhanced monitoring” of people with respiratory illnesses will continue, per international standards, set by the World Health Organisation, the Pan American Health Organisation and the Caribbean Public Health Agency. Ms Wilson added: “The public is advised to act on the recommendations of the ESU.” Travellers who have been to China, ground zero of the outbreak, or areas known to have human-to-human transmission of the virus, known as 2019-nCoV, were advised to “identify yourselves upon arrival to customs and immigration officials, who will provide you with a health information card for follow up if necessary”. A government spokeswoman told travellers: “If you are ill upon arrival, inform airport personnel for assistance.” The spokeswoman added: “If you become ill with a respiratory infection following travel to China or another affected region, call your healthcare provider in advance, inform them of your travel history and seek medical care.” Residents are advised to avoid non-essential travel to China and other places where there have been confirmed cases of human-to-human transmission. The public was also told to ensure their immunizations were up to date. Health experts said people should also regularly wash their hands, use safe food handling practices and avoid contact with people that have respiratory infections, as well as farm and wild animals. People who have no travel plans are advised to take medicines as prescribed, cover their mouths when they cough or sneeze and to stay away from work and social gatherings if they are ill. At least 82 people have died in China from the virus, which has also infected at least 2,900 worldwide. Cases of the virus have been confirmed in Hong Kong, Macao, Taipei, Thailand, Vietnam, South Korea, Singapore, Malaysia, Japan, Australia, France and the United States. A spokeswoman for Bermuda Hospitals Board said today: “Following the recent advisory by the Ministry of Health regarding the coronavirus — 2019-nCoV — that was first identified in Wuhan in China, BHB can confirm that even though the current threat to Bermuda residents is low, we are closely monitoring developments and are ready to respond should the threat increase. BHB has questions in its admission process that identifies anyone who has travelled to a place where there have been known infections and we are ensuring we have all necessary supplies. BHB has protocols in place as part of day-to-day running of the hospitals to minimise the spread of infectious diseases. Measures include negative pressure rooms in the emergency and the acute care wing units that are checked daily and infection prevention protocols, such as using protective equipment and clothing. We also have plans in place that enable us to deal with outbreaks and epidemics that could be triggered if the mode of transmission changes and global infection rates continue to increase.” Michael Ashton, BHB’s Chief of Medicine and Infectious Diseases Specialist, added: “We are closely monitoring this novel coronavirus and continue to work closely with Government. BHB has detailed plans for dealing with outbreaks and epidemics and we swiftly reviewed our admissions processes as a precaution. We would ask that people only come to the hospital emergency department if they truly have an emergency situation. If you are concerned that you may be infected, please call your family doctor or the emergency department before you arrive — as people in the same waiting area could be otherwise put at risk.”
2020. January 28. Legal action to keep the six-figure salaries of its top executives a secret has been launched by the Bermuda Hospitals Board.
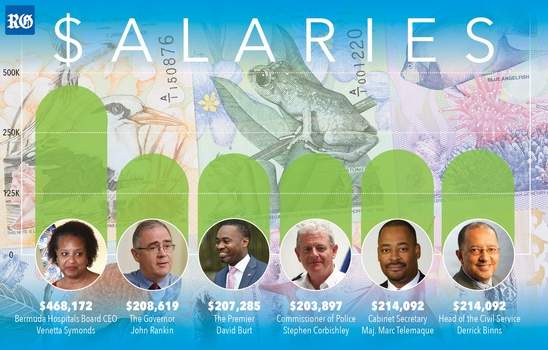
Graphic above reveals how hospital chief earns for more than top Government officials.
The board, which will receive almost $146 million in public funds this financial year, said it could not comment on how much the litigation is likely to cost. The court move came after the BHB was ordered by Information Commissioner Gitanjali Gutierrez on October 31 last year to disclose the total cost of each position in its executive team, within $10,000 bands, for the financial year 2015-16. Ms Gutierrez’s decision followed a public access to information request filed by The Royal Gazette in January 2016, which was twice rejected by the BHB. The commissioner said the salaries and other details of compensation should be shared with the public in the interests of “accountability and transparency” and gave the board until December 12 to disclose the amounts. But the BHB, represented by law firm Conyers Dill & Pearman, filed an application for a judicial review in the Supreme Court on December 11. The court suspended Ms Gutierrez’s order on December 17 pending the outcome of the case. Ms Gutierrez told The Royal Gazette: “In light of this, I will not enforce the order of October 31, 2019 at this stage.” A BHB spokeswoman said: “Bermuda Hospitals Board is following the process for reviewing a decision of the Information Commissioner, as set out in section 49 of the Pati Act. Out of respect for this legislated process, our concerns will be fully heard at the judicial review hearing.” The spokeswoman added that the BHB was “unable to say what the legal costs will be at this point in time, as the amount will depend on whether the matter will be contested. The final cost would also depend on how long any hearing would last and the outcome. If the BHB prevails, then its costs will be reimbursed. BHB determined that it did not agree with the decision of the ICO and ultimately there will be final guidance from the court on the matter. The ICO must follow the law, as must BHB, and where there is dispute, then this is the process which will allow a fair and final determination.” The BHB revealed in May 2016 that chief executive and president Venetta Symonds’s basic pay was $468,172 and total compensation was $469,979. The total cost of Mrs Symonds’s position, including leave-pay provision, social and health insurance payments, payroll tax and pension arrangements, was $504,179. But the hospitals board did not release full details for the six other executive team members, the chief of staff, chief financial officer, chief operating officer, chief of nursing, chief of psychiatry and the Mid-Atlantic Wellness Institute’s chief operating officer. The board said only that each employee’s total cost ranged between $158,300 and $504,000. Ms Gutierrez said in her decision that the range given by the BHB in its May 2016 disclosure was “very broad”, so much so that it did not “further the accountability purposes of the Pati Act”. She said it resulted in instances in which the cost for executives was less transparent than for employees at the middle and junior levels. David Burt, the Premier, picks up a salary of $207,285, according to the latest Government Budget Book and the Cabinet Secretary and Head of the Civil Service each get $214,092 a year. Government House said the Governor’s annual salary was $208,619 and Government’s compensation list on its website said Commissioner of Police Stephen Corbishley was paid $203,897. The board claimed during Ms Gutierrez’s review that more detailed compensation information would erode senior staff’s right to privacy and give candidates who applied for executive positions a competitive advantage in salary negotiations. The BHB also said disclosure might cause prejudice against the officials in a “micro-community” such as Bermuda, and claimed it put the executives in a prejudicial position as no other senior executives on the island were required to have their total compensation packages disclosed. The Information Commissioner’s decision highlighted that hospital executives in Canada and in Britain had their actual salaries or salary ranges available to the public. The commissioner said that in Bermuda “a number of senior executive posts have an associated actual salary published, not salary range”. Ms Gutierrez continued: “It is unclear how BHB salary executives would have more challenges with public accountability for their salary ranges than any other senior executive in the public sector, whose salary range or salary is published in a proactive manner for the public, or is otherwise disclosed in response to a Pati request. The executive team members hold the most senior executive positions within BHB. It is reasonable to expect these executive team members to have less expectation of privacy concerning their compensation. These individuals are accountable to the public for the management of Bermuda’s only hospital facility. The governance and management of BHB by the executive team also has a direct impact on how the public funds received by BHB are spent. BHB’s claims of discrimination or prejudice against its executive team members appear to be speculative, as no support was provided for those claims.” The commissioner’s order required disclosure of the total cost, within a range of $10,000, for each executive team position, along with records related to payments for social and health insurance, payroll tax and pensions. Ms Gutierrez also ordered disclosure of a list of payments made by the BHB to professional services firm PwC during the financial year 2015-16 for an interim CFO (see separate story below). Ms Symonds is due to retire as BHB CEO and president in July. Craig Rothwell, of law firm Cox Hallett Wilkinson, represents the Information Commissioner’s Office in the judicial review. He confirmed that Ms Gutierrez would contest the judicial review and said a hearing date was still to be set.
Venetta Symonds, who retires in July, became CEO in April 2012. Her predecessor was David Hill.
2020. January 24. The husband of a young mother who had terminal cancer diagnosed days after their son was born won $1.9 million in damages yesterday for medical negligence from the Bermuda Hospitals Board. Chief Justice Narinder Hargun ruled that Kemar Maybury deserved the award because his wife, Latifa, would have been “treatable for cure” for colorectal cancer if an emergency room doctor at the King Edward VII Memorial Hospital had not failed to detect a rectal tumor and if the hospital had not failed to ensure that faxed medical notes were received by the patient’s GP. But Mr Maybury’s legal battle may not be over because the board’s lawyer, Allan Doughty, told the Supreme Court: “My client is very serious about appealing this matter.” A BHB spokeswoman said last night no decision had been made on an appeal. She added: “BHB will decide on its response following a full review of the judgment, within the time allowed for such consideration.” Mr Maybury, who lost his wife in November 2013, only six months after son Khaleel was born, was not in court for the judgment. His mother, Keetha Lowe, who is helping to raise her six-year-old grandson, was present. “It’s been a seven-year battle. Khaleel is in his seventh year,” she said. “He is asking for questions to be answered and I can’t answer Khaleel’s questions in a way that a seven-year-old would understand. I am tired. I really want to put it to rest. I really want to put Latifa to rest and, to a significant degree, I want to put Bermuda to rest. This case has not just affected our family but the entire community.” Ms Lowe fought back tears as she added: “Latifa was an only child and her mother is still having to face the realities of what’s occurring right now.” She said the case was a chance for the BHB to admit there was something “critically wrong with its policies and procedures” and own up to failures in its standards of patient care. She added that the BHB had decided to engage in “fierce fighting” against a grief-stricken family. Ms Lowe said: “When not even death moves authorities to do the right thing, then the community as a whole is at risk.” The BHB admitted to the court that it was a breach of its duty of care when emergency room doctor Jacquiline Bisasor- McKenzie misdiagnosed Mrs Maybury with internal hemorrhoids in August 2012 after she went to the hospital with rectal bleeding and stomach pain. It also admitted it was in breach of its duty when it failed to ensure a faxed copy of Dr Bisasor-McKenzie’s discharge summary, which included a follow-up instruction for Mrs Maybury to be referred to a specialist for a colonoscopy, was received by her GP. But the board argued that even if the right diagnosis had been given it would have made no difference to the outcome given what it claimed was the “advanced staging” of the cancer in August 2012. Mr Justice Hargun disagreed and highlighted he had seen no evidence that cells from the primary tumor had spread to Mrs Maybury’s lymph nodes at that time. He accepted the evidence of expert witness Michael Leitman, a surgical cancer specialist who is chief of general surgery at Mount Sinai Hospital in New York, that “had Mrs Maybury been correctly diagnosed in August 2012, Mrs Maybury’s condition would have been treatable for cure”. The Chief Justice said: “In this regard, I accept Dr Leitman’s evidence that her chances of survival were up to 60 per cent.” He wrote in his judgment: “I am clearly of the view that the expert evidence of Dr Leitman was that had proper diagnosis been made in 2012, Mrs Maybury would have been cured from the cancer. The clear implication of Dr Leitman’s evidence is that she would have a normal life expectancy.” Mrs Maybury, originally from Morocco, had just turned 30 when she died. She and her husband married in 2010 and settled in Bermuda. Then they ran the successful Smokin’ Barrel food truck, which has now gone out of business. Her health problems began in May 2012 when she started to suffer from constipation and rectal bleeding. Ms Maybury reported rectal bleeding and abdominal pain for the previous three months at the August 2012 visit to the ER and was given suppositories and an X-ray. The judgment said: “The rectal bleeding continued but Mr and Mrs Maybury took comfort in the fact that Dr Bisasor-McKenzie had diagnosed the condition as internal hemorrhoids. “They did not receive any further communication from their GP ... following the visit to the emergency department ... They had no reason to suspect that the discharge summary may not, contrary to their understanding, have been faxed to [GP] Dr [Shaina] Kelly.” Mrs Maybury returned to the ER in December 2012 when 18 weeks pregnant and again in January and April the following year. Khaleel was born a month early by Caesarean section on May 9, 2013 after “an obstruction to normal delivery” was discovered. Mrs Maybury was diagnosed days after the birth with terminal colorectal cancer, which had spread to her lymph nodes, liver, lungs and spleen. Jai Pachai, who appeared for Mr Maybury, told the court the patient suffered “excruciating and ongoing pain and suffering” before she died on November 18, 2013. Ms Lowe praised Mr Pachai for his work on the case. The damages award included amounts for pain and suffering, bereavement, and loss of maternal and spousal care. But Ms Lowe said: “Let’s be honest, no amount of money returns a mother to her child and to her husband and to her family at a time when she should be here. No amount can compensate for that.” She added that the BHB “have to fight this as much as possible to avoid setting a precedent for others to follow and, Lord knows, there’s more than enough to follow”. The BHB spokeswoman said: “In response to today’s judgment, while we strive to do our best each day caring for all people who come through our doors, we are truly saddened by the outcome for Mrs Maybury and sorry for where our service failed her and her family back in 2012. Since Mrs Maybury’s experience, BHB has worked to improve the communication between the hospital and community physicians by offering highly secure BHB e-mails through which patient information, such as emergency discharge sheets, can be confidentially shared. BHB is working collaboratively with Bermuda Medical Council and doctors to determine the most effective solution to this complex communication problem between all care providers. “In the near future, this will include sending family physicians a daily list of all their patients who attended the emergency department, with a follow-up telephone call to ensure the list was received. Further ahead, BHB hopes the implementation of an electronic medical record will provide a platform to significantly progress towards a community solution.”
2019. December 19. Work to eliminate mother-to-child transmission of HIV and syphilis means Bermuda held its place among a small group of countries to be internationally recognised for the achievement. The Ministry of Health revealed today that the island was revalidated with EMTCT status after its initial certification in June 2017. It added that the status was a “prestigious public health accomplishment” achieved by only 11 countries worldwide. Kim Wilson, the Minister of Health, said: “We were delighted and very proud of that achievement. However, once achieved, EMTCT must be maintained. EMTCT validation indicates that Bermuda is proficient at preventing mother-to-child transmission of these infections. Good antenatal care, early testing for HIV and syphilis and treatment for HIV positive mothers can prevent transmission of HIV from an HIV-positive mother to her infant during pregnancy, labour, delivery, or breastfeeding. However, HIV remains a threat and complacency is especially dangerous. Both HIV and congenital syphilis have serious implications for the lives of babies and can be prevented. Hence, the importance of maintaining elimination status.” The ministry explained that validation of elimination status was made by a special committee of the World Health Organisation, which assesses a country’s systems to check for HIV and syphilis in pregnancy, its laboratory capacity for accurate testing and access to antenatal care for all adolescents and women. The committee also looks at private and public healthcare collaboration as well as care quality. Countries must demonstrate to Global Validation Advisory Committee standards that the country’s programmes and procedures can be relied upon to identify early and treat cases of the diseases during pregnancy. The standards do not require that the conditions are absent in a community, but countries must show that pregnant women are adequately tested and cared for. Programme indicators confirmed that in Bermuda more than 95 per cent of pregnant women are tested early in pregnancy for HIV and syphilis. To meet the requirement for both diseases, a country must show:
Ms Wilson said: “In September, Bermuda sent the required maintenance report to GVAC. Our report indicated both the processes used in Bermuda to assure all babies and mothers are tested for HIV and syphilis and provided necessary treatment to prevent mother-to-baby transmission. In addition, we provided feedback on how Bermuda had responded to the recommendations made by the committee during the initial validation visit in June 2017. In order to prepare a maintenance report required an enormous amount of work on the part of the ministry to collect data from Bermuda Hospitals Board, Register General and Epidemiology and Surveillance Unit. We are particularly grateful for the generous collaborations with Department of Health and BHB professionals who played a critical role in this achievement by providing an enormous amount of clinical information.” The ministry said that the GVAC told health officials this month that Bermuda was “in a very strong position to continue to maintain validation of EMTCT of HIV and syphilis”. It highlighted the island’s “strong expertise and commitment” to the elimination of mother-to-child transmission of the diseases and commended Bermuda for “these national, regional and global achievements”. The next review for maintenance of validation of EMTCT will be September 2021.
2019. December 10. Changes to the healthcare insurance system will go ahead, despite a call from the Opposition to put the plans on hold, the Government said yesterday. The Government added it would not extend the consultation period on the changes — which ended on Sunday. Kim Wilson, the Minister of Health, said: “In August of this year we undertook to conduct a comprehensive public consultation period on the Bermuda Health Plan. “In the four months of open, transparent consultation over 50 meetings were held with over 600 participants. I am confident that this period has allowed ample time for the public to provide feedback on what the core insurance plan should include and how to transition to a more efficient health financing system.” Pressure group Patients First and the Opposition have both criticized the proposed changes asked for more time to look at the plans. But Ms Wilson said: “I appreciate that Patients First and the Opposition are asking for the Government to do a U-turn on its decision to adopt a unified model of health financing or a single payer system. Unfortunately, their campaign has deliberately misled the public with numerous misstatements, leading to confusion and fear. As a Government, we have to act in the best interest of the people and we have to make decisions that will benefit the whole of Bermuda not just those with vested interests.” The Minister added the Progressive Labour Party had an electoral mandate to pursue universal health coverage and tackle the high cost of healthcare in Bermuda. She said: “Bermuda is a small jurisdiction and our health financing system unduly complicated, expensive and unsustainable. We have to find ways to minimise co-payments, improve access to primary care, and offer benefits to restore people’s health and we are confident that simplifying our fragmented health system will help put us on the road to sustainability. Much work remains to be done on the Bermuda Health Plan and working groups will be set up to consider the public feedback and determine next steps.” She was speaking after the One Bermuda Alliance asked Government to take a step back after concerns were raised over the plans. Patricia Gordon-Pamplin, the Shadow Minister of Health, said: “An Age Concern meeting on the health plan was left with standing room only and about 6,000 people have signed a petition against universal healthcare. The Minister insists that this is not rushed, and she has referred to a report which was done in a bipartisan way in 2012, thereby insinuating that the public has had seven years to digest this policy. The reality is that the report was not a bipartisan report, it was a sub-committee report issued by interested stakeholders. There were no public meetings explaining the changes or their impact on the public.” Ms Gordon-Pamplin added: “The OBA supports healthcare reform because 60,000 people spending $700 million a year is not sustainable, but clearly Bermudians are very concerned about Government’s plan and it must put it on hold until more details such as a true cost and details of all benefits are available.”
2019. December 9. A professional services firm has been recruited to help deliver a joint vision for a healthier Bermuda, the Government announced last night. KMPG will provide project management as the island’s “health strategy” is updated. It came as public consultation on health financing reform ended yesterday. Kim Wilson, the health minister, said: “We all want affordable and high-quality healthcare. Together, we are working hard to ensure all residents enjoy equitable access to the quality care our families depend on, while making important choices to put our healthcare system on a sustainable path.” She explained that the Bermuda Health Strategy 2014-2019 was published under former health minister Jeanne Atherden, during the previous One Bermuda Alliance government. Ms Wilson said it built on the earlier National Health Plan and “outlined strategic reform priorities for Bermuda’s health system”. She added: “Much was achieved since that time, but further work is required to fully achieve success. With the strategy expiring this year, I want to build on that good work and refresh and upgrade the Bermuda Health Strategy to produce the vision and goals for 2020 to 2025. We are determined to make Bermuda healthier and we need a joint vision for health that inspires hope, trust and confidence across the community. This project will be led by a multisectoral steering committee and a broad cross-section of healthcare stakeholders as a Strategic Leadership Group. Their input and guidance will set the direction of the 2020-2025 strategy for healthcare in Bermuda. Further, to support our efforts, we have engaged KPMG to provide independent, local project management resources and to leverage their global healthcare insight. KPMG has been engaged via a partnership between the Ministry of Health and the Bermuda Hospitals Board.” Ms Wilson said that BHB believed in the need for a “comprehensive and shared strategic vision and plan for Bermuda”. Members of the health financing reforms stakeholder consultation group, which was set up last year, were invited to take part in the Strategic Leadership Group along with other health professionals. Consultation with relevant groups will take place in the first quarter of 2020. Short surveys — to be carried out and analyzed by KMPG — were expected to be launched this week on forum.gov.bm. Ms Wilson said: “The Strategic Leadership Group will guide the way to build consensus on the current state of healthcare in Bermuda and the future state that we want to achieve together. Bermuda has a strong and compassionate healthcare system. This is the result of tremendous effort from our frontline providers — our dedicated doctors, nurses and allied health professionals — and the business community, insurance sector and Government. I believe this broad stakeholder collaboration will assist my ministry by bringing the breadth of perspectives across healthcare leaders in our community. I look forward to the outcome of their deliberations to provide me with the 2020-2025 vision for healthcare in Bermuda.” The Bermuda Health Strategy takes in the wider health system including prevention and long term care. The Bermuda Health Plan is a part of the broader strategy and is focused on health financing reform to improve access and sustainability in the health system.
2019. December 2. Bermuda Hospitals Board (BHB) has achieved a decision of Accredited with Exemplary Standing, Accreditation Canada’s highest level of accreditation. The decision follows four years of quality and safety improvements, culminating in a weeklong onsite visit by independent surveyors in May. Accreditation Canada is a non-profit organisation that works with the Ottawa-based Health Standards Organization, healthcare providers, policy makers and patients to improve the quality of health and social services. More than 1,000 health and social service organisations and 7,000 sites around the world have been accredited by Accreditation Canada with a goal of safer, high-quality healthcare. Accreditation Canada surveyors are volunteers who are healthcare professionals in senior clinical or administrative roles at other accredited organisations. BHB CEO and President Venetta Symonds said: “I’m very proud of this result, which reflects the dedication and hard work our staff devotes to BHB’s quality and safety improvement projects in addition to their daily work of caring for our patients. The surveyors emphasised how much we’ve achieved at BHB over the last few years, and even in the six months prior to the survey. They applauded how we have used the Strategic Plan 2016-2021 at the centre of our planning across BHB, and how our extensive Clinical Services Plan serves as the anchor for our strategic goals. They cited our dedication to quality and safety improvement and training at all levels, especially initiatives like the introduction of daily bullet rounds on inpatient wards and more focused discharge planning, the significant reduction in pressure injuries, our commitment to early identification and treatment of sepsis, and our increasing engagement of patients and families in policy and process development. They recognised the involvement of our entire team in achieving these results.” BHB Chief of Staff Michael Richmond, MD, said: “In Bermuda our hospitals are required by law to be accredited by an approved accrediting body. However, the most important part of the process is the opportunity to receive feedback and recommendations from the Accreditation Canada team and the surveyors based on the knowledge and insights they’ve gained from our peers across North America and around the world. Clinical and non-clinical teams across BHB have been collaborating with the Institute for Healthcare Improvement, Johns Hopkins Medicine International and other partners to identify and implement changes to our services, processes and policies. These changes are already having a significant impact on the quality and safety of our care, as evidenced by Accreditation Canada’s survey findings.” Mrs Symonds added: “Achieving the highest level of accreditation does not mean we don’t have more work to do. The survey report highlights the things we’re doing well, but it also outlines areas we need to improve. Their advice, along with our other quality improvement partners, will help us along the journey to attaining our vision of Exceptional Care. Strong Partnerships. Healthy Community. One of our greatest resources on this journey is our patients and their loved ones. Their input on our services and care is invaluable in identifying the areas we fall short and helping us deliver the best possible care to every patient, every day. Our newly formed Patient and Family Advisory Council also provides advice on how we can implement or change processes to improve the patient experience. Thank you to the Council and to every member of the community who has taken the time to contact our unit managers and patient relations with their suggestions and concerns.” From 13-17 May 2019, four independent surveyors assessed BHB against 26 sets of healthcare standards, 35 priority processes and 30 required organizational practices. They spent time at King Edward VII Memorial Hospital, Mid-Atlantic Wellness Institute, Lamb Foggo Urgent Care Centre and three of BHB’s group homes, observing staff, reviewing documentation and policies, and interviewing staff, patients and community partners. The surveyors’ findings were then reviewed thoroughly by the Accreditation Canada team before an accreditation decision and full report were issued. “Accreditation Canada is committed to supporting organisations like Bermuda Hospitals Board, who offer safe and effective care with a focus on continuous improvement. We commend BHB for their outstanding achievement and their contributions to our goal of achieving quality health services for all,” noted Katerina Tara ova, Accreditation Canada’s executive director of international accreditation. Accreditation Canada will continue to work with BHB throughout the four-year accreditation cycle, reviewing evidence related to unmet criteria, providing feedback, and monitoring standards and practices to ensure the organisation continues to perform at the expected level. BHB has been accredited since the 1970s. This year marks the 13th onsite survey by Accreditation Canada. The next survey will be held in May 2023. The accreditation report, decision letter and survey comparison table are available on the BHB website at bermudahospitals.bm.
2019. November 28. Almost 3,000 people have signed a petition to demand that controversial proposals to change the way health insurance is funded are scrapped. The petition against the Bermuda Health Plan was set up just after a public forum that called for the proposed changes to be taken off the table. But a health ministry spokeswoman said last night that a four-month public consultation period had given “good time for the public to participate in the discussion”. She was speaking after Patients First, a group of doctors in the Bermuda Medical Doctors Association, launched a change.org online petition against the proposals on Tuesday night in the wake of a town-hall meeting that criticised the plan. The Bermuda Health Plan was designed to pool all the island’s residents in one unified health insurance package. That would replace the present Standard Health Benefit, which is paid into by private insurance companies to cover health costs. The ministry argued that a health insurance pool would be more efficient and share costs across the island’s residents. Henry Dowling, the president of the BMDA, said the proposed changes would create a monopoly in health insurance that would also hit the quality of care and fail to reduce healthcare costs. But the health ministry spokeswoman insisted: “Bermuda’s population is small from an insurance pool perspective. With insurance it’s the law of big numbers that makes a difference in managing risk.” She added: “The standard health benefit is already in a virtual single pool and the premium has been community rated since 1970. Like many public goods, this is not about a monopoly or a market, but about how effectively it is regulated and how well it serves the population.” She said the Bermuda Health Plan wanted to create “a larger, more efficient risk pool that will create a sustainable platform to improve access and sustainability in our health system”. The ministry said that more than 45 meetings were held on the reforms with more than 500 participants and public views continued to be sent to the email address healthplan@gov.bm. The spokeswoman added: “The feedback we are hearing will inform the next stage of the process when working groups will be set up to digest recommendations on how we should proceed.” The wide-ranging healthcare changes are expected to be launched in the autumn of next year.
2019. November 28. The maximum allowed waiting time for routine medical imaging services has doubled from three weeks to six weeks at King Edward VII Memorial Hospital because of funding changes, The Royal Gazette can reveal. New imaging services triage guidelines said a move to a $330 million government grant instead of a fee-for-service arrangement had forced an end to weekend overtime in the scanning services unit if the waiting list for routine procedures was over the three-week limit. But a Bermuda Hospitals Board spokeswoman said waiting times were still “well below” the six-week limit and patients were getting a better value service. The changes came into force on July 15. The document that outlined the new rules said: “For the last few years and prior to the cap, we have opened on weekends once we saw a backlog extend close to three weeks. These operating hours were achieved by staff overtime funding as they were supplementary to normal shifts. We can no longer sustain these expenses with the current cap as all departments across BHB are mandated to reduce overtime.” The document, dated July 10, expanded the time requirement for routine appointments — the lowest on the urgency scale — to six weeks, and asked for them to be “distributed throughout the community imaging clinics” when possible. More urgent cases had shorter waiting times under the triage policy. Emergency scans must be performed inside six hours, high-priority scans within two days and intermediate priority cases must be scheduled for between one and two weeks. The document said that, at the time of writing, there was a four-week waiting time for routine MRI scans and two weeks for routine CT scans at the hospital. It added: “Four-week wait times for patients requiring routine examinations is acceptable as most major jurisdictions measure wait times based on volumes in excess of six weeks. The objective of the new triage guidelines is to ensure that the KEMH Imaging Services Department reserves appropriate capacity to accommodate the true demand by clinical need.” Doctors were also asked not to bump patients to a higher priority because it could affect the treatment of patients who were genuine urgent cases. The document warned: “Diagnostic Imaging will address physicians that abuse the system.” The BHB spokeswoman added: “The absolute maximum wait for routine appointments is six weeks, but our current wait times are well below this at BHB — and we are doing all we can to maintain and even improve these. Alongside the new guidelines circulated in July are a number of initiatives aiming to improve efficiencies within the BHB Imaging Services department with the goal of reducing wait times and costs. Diagnostic Imaging utilization is now at 68 per cent rather than 53 per cent compared to last year. This means the community is getting a better value service that is meeting high quality standards. The grant that BHB now works under requires us to innovate and improve efficiency, but this is only done where international standards of quality — including wait times for services — can be met. Overtime is sometimes required, and our plans to ensure it is only used when needed do not necessarily mean reducing service access. Updating schedules can also reduce overtime with more appropriate staffing of services.” She said that overtime had been used in the past to reduce the waiting time for routine appointments to 48 hours, but that that time frame was not clinically supported as an international standard. Since the start of the new guidelines the average wait times for some imaging services had increased and others had fallen. The average waiting times for CT scans dropped from 14 days in June to 11 days in October and the wait for ultrasounds plummeted from 29 days to five days over the same period. But the wait for mammograms rose from one day to 12 days, the wait for MRI scans increased from 14 days to 17 days and the wait for nuclear medicine scans doubled from six days to 12 days. The average waiting period for radiology, bone density scans and interventional radiology have remained unchanged. Allan DeSilva of the Bermuda Healthcare Advocacy Group said he had not heard any complaints about delays in scans since the new policy was introduced. But he said that any delays could affect patients. Mr DeSilva added: “Most people take these things for granted. You might not think that 13 or 14 days is a long time, but it can be if you are a patient.” A spokeswoman for the Bermuda Cancer and Health Centre said: “From our perspective, the waiting times for diagnostic imaging used to determine a cancer diagnosis and staging remain minimal and within acceptable standards. Overall, the BHB wait times reported seem reasonable as change is being implemented. At this time it is too early to see the long-term impact.”
2019. November 27. A rallying cry went out last night from opponents of the Bermuda Health Plan 2020 to shelve the Government’s proposed reforms. A packed house at a forum by the pressure group Patients First was urged to join a petition turning down “rushed” changes that would lead to a government-enforced “monopoly” on health. Henry Dowling, president of the Bermuda Medical Doctors Association, revealed the petition after a cancer patient in the audience asked: “How are we going to stop this from going through?” Saying she had cancer diagnosed twice, and that “most insurance companies won’t touch me”, she added: “If other people can march and stop things from going through, why can’t we all do something to stop this?” Dr Dowling told the forum that the physicians’ group had met two weeks ago with David Burt, the Premier, to air its concerns. The BMDA head added: “He believes this is in the best interests of the people — so the people need to speak and let him know they do not believe this is in their best interests.” The panel also included Janie Brown, a dentist, Jamie Burgess, an optometrist, and Stephen Kenny, a pediatrician and economist. Nearly 300 gathered at St Paul AME Church Hall, with the December 8 deadline for public consultation on the health proposals drawing near. Dr Dowling repeatedly described the proposals for a unified healthcare payment system, revealed in August by health minister Kim Wilson, as a monopoly. He added: “We know that any one thing having all the power is a dangerous system to have, and I don’t care who it is.” Dr Dowling said the proposal failed to address the $730 million spent annually for about 60,000 people, adding: “This system does not fix that. All it does is shifts who pays for it.” He called on patients to “take back control” and make their voices heard, while Dr Kenny warned that in a system without competition, “the product becomes worse”. Dr Kenny also cast doubt on the minister’s suggestion this summer that the plan could be delivered at a cost of $514 a month per adult. He told the forum: “Some higher amount than that will only be disclosed when there’s two weeks of consultation left — soon, I hope.” He said there was “overwhelming opposition” to the plan among the BMDA, even though physicians would not lose out in payments. “Our opposition is not a financial one,” Dr Kenny said. “Our opposition is that we think it’s bad for patients.” But the meeting also heard of pitfalls to earlier healthcare payment changes that were approved by Parliament in May. The change mandated that the Bermuda Hospitals Board would receive a $330 million annual lump sum from the government. The grant replaced the previous fee-for-service arrangement under the Health Insurance Amendment Act. Dr Brown said this switch had “wreaked havoc” at the hospital, causing the closure of two operating theatres because BHB was “trying to save money”, and leading to delays in elective surgeries. She said the grant had been given without guidelines to the hospital on “how to manage the money or spend it”. One audience member told the panel: “Anything we should be concerned about, it’s got to be healthcare. How broad is the conversation? It doesn’t seem broad to me — it’s Government and doctors.” Dr Burgess said that in spite of three months’ consultation, including three town hall meetings offered by the ministry, many patients still “do not have a clue what’s going on”. She added: “There is, unfortunately, a lot of confusion.” Dr Dowling said the Government had failed to heed doctors’ concerns. He added: “You need to listen to us. We represent the soldiers on the ground. You have to just listen to us before you get the whole war lost. That’s all we are saying here.” A woman retiree complained about inconsistencies in the co-pay that seniors were having to cover, telling the forum there was “a total disconnect between the medical industry and the patients”. She described getting charged a copay of more than $200 last month “just to have a doctor look inside my mouth”. She said: “It’s very humiliating to have to say you can’t afford it and you can’t pay this. It’s just got to get better. I wish we as consumers could be involved more.” She added: “There seems to be a huge disconnect between customers and the industry as a whole. Government is acting as Government — they are not taking the responsibility that they need to take.” The forum closed with a call for the public to petition the Government over the Bermuda Health Plan via the Patients First page on Facebook. A petition was also online at website change.org. By 9pm, it had been signed by nearly 200 people.
2019. November 26. The health minister will not attend a public forum organised by a pressure group about the Bermuda Health Plan today. Kim Wilson, the Minister of Health, said she was pleased by the level of public involvement in the debate on the future of Bermuda’s healthcare, but that she would be overseas on government business. She said: “It is regrettable that I am not on island to participate in this important town hall by Patients 1st Bermuda. I hope it generates the fruitful dialogue we have seen from most stakeholders, so we can continue to receive constructive feedback to improve access and sustainability for all of Bermuda”. The meeting, to be held by Patients 1st Bermuda, was organised to let the public hear the perspective of medical professionals on proposed healthcare reforms. Several people scheduled to take part as panellists are doctors, including Henry Dowling, president of the Bermuda Medical Doctors Association, Steven Kenny, a pediatrician, Janie Brown, a dentist, and Jamie Burgess, an optometrist. The Patients 1st Facebook page said: “We think Bermuda healthcare is too expensive. Healthcare reform is good. #Rushedhealthreform is not good. Patients 1st wants the Government to postpone all health reform legislation until they can tell us in real terms what the financial impact will be for Bermuda’s workers and families.” The meeting will be held at the St Paul AME Centennial Hall in Hamilton at 5.30pm.
2019. November 25. Proposed changes to the healthcare system in a bid to cut its massive costs without proper information would be a disaster, the head of a think-tank has warned. Philip Butterfield, the chairman of the BermudaFirst advisory group, said healthcare at present was “not sustainable”. But he added: “The pursuit of a single-payer approach in the absence of detailed data about the endgame is a recipe for, in our judgment, confusion, discord and unintended consequences, and I feel that it is going to fracture our community. This needs to be avoided at all cost. It is important that we not retreat to tribalism, the issue is far too important.” He added that the Government should recruit international experts to help make the necessary changes to healthcare. Mr Butterfield said: “It is the Government’s largest expenditure. BermudaFirst supports a holistic approach to this critical issue and believes that it is necessary to obtain external, globally recognised expertise to assist us in developing a multi-faceted solution to this challenge.” Mr Butterfield was speaking at an Association of Bermuda International Companies lunch last week. Kim Wilson, the Minister of Health, who has announced a proposed move to a single-payer healthcare system, said she supported the use of overseas experts to develop changes. She added: “I’m happy to remind the public that the pursuit of the single-payer option, or a unified health financing system, for a core benefits plan followed extensive considerations by local and international experts ...” Ms Wilson said that the health finance options were developed by a bipartisan task force made up of insurers, employers, healthcare providers, an overseas actuarial firm and Marc Roberts, the professor of political economy and health policy emeritus at the Harvard School of Public Health, who prepared a 100-page report. She added that Professor Roberts had assisted government in more than 30 countries over his career and had written seven books and a string of articles on healthcare reform, including Getting Health Reform Right: A Guide to Improving Performance and Equity. Ms Wilson said: “Following these detailed considerations, the Government decided to adopt the unified model as the most efficient for our small jurisdiction. Following the current public consultation period, working groups will be established to consider the feedback and develop recommendations; and we plan to further engage local and international expertise at that time.” Doctors have launched pressure group Patients First Bermuda which claimed the government’s draft Bermuda Health Plan 2020 would lead to more underinsured and uninsured residents and could force medical practices to close.
2019. October 28. Discontent voiced by doctors at an event on healthcare reform demonstrates mistrust of the Government, the shadow health minister said yesterday. Patricia Gordon-Pamplin said: “It was very clear to me that doctors were expressing their concern and frustration at being dictated to, under the guise of consultation. There clearly has not been a meeting of the minds in respect of how the proposed changes will impact the doctors who are an integral part of this entire process.” She was speaking after a town hall meeting was held in the East End last week to discuss changes to healthcare coverage in Bermuda. Kim Wilson, the Minister of Health, announced in August that the Bermuda Health Plan 2020 was to replace the Standard Health Benefit coverage for all island residents. The level of coverage that will be provided and who will administer the scheme have not been determined. Ms Wilson said in August that there would be a four-month consultation period on what the plan should include and cost. The most recent town hall meeting on the proposed change was held at Penno’s Wharf last Thursday. Ms Wilson was joined at the event by Jennifer Attride-Stirling, the Permanent Secretary of Health, and Ricky Brathwaite, the acting chief executive officer of the Bermuda Health Council. The 75-minute meeting included a question-and-answer session. Several times during the session answers were interrupted by reactions from the crowd. Anthony Richardson, a Progressive Labour Party senator, was at the event. He said in an op-ed released at the weekend that he was “utterly shocked” by the behaviour of some doctors who attended. Mr Richardson said that the doctors had “attended en masse, without declaring their presence”, and had “booed and heckled”, Ms Wilson, Ms Attride-Stirling and Mr Brathwaite. He added: “They are prepared to hold Bermuda for ransom. I thought they were here for the patients and not the money.” Mr Richardson said that doctors had been unwilling to listen to the event’s speakers who had repeatedly said that consultation on the proposed reforms was ongoing. He added: “They insisted on speaking and behaving as if it was all a done deal and there was nothing more to discuss. They refused to accept facts regarding existing health insurance laws and published data on insured headcounts.” Mr Richardson said that it was “truly sad to see this side of doctors”. He added: “Thankfully, we know that not all doctors are like that as it is only the vocal angry ones whose greed and self-interest drives them to put profit before patients, and to favour fiction over facts. We know that there are plenty of good doctors who don’t share this perspective. Mr Richardson added: “They have patient health at the forefront of their minds.” Ms Gordon-Pamplin said that doctors would have been “considered remiss” if they had not attended the event. She added: “They attend, and they are criticized. Whereas the senator has an obligation to express his support for his Government’s position, the doctors have a responsibility to their patients to ensure that what is being driven by the Government will not have a negative impact on the level of care. Everyone does not roll over and play dead when the Government speaks, and the lack of clarity so far is creating anxiety.”
2019. October 15. The Ministry of Health has advised that the town hall meeting scheduled for Thursday has been postponed. A new date for the St. George’s town hall will be announced shortly. The public is encouraged to review the proposed Bermuda Health Plan. The Ministry of Health welcomes feedback on the proposed plan.
2019. October 14. The former chief executive of the Bermuda Health Council will consider her next steps as she battles a government that seems to have bottomless pockets, her lawyer has claimed. Eugene Johnston, who represents Tawanna Wedderburn, said her legal proceedings against the Premier, the health minister, the health council and its former chairwoman were just beginning, despite a ruling last week that found her case could not be tested by judicial review. Assistant Justice David Kessaram found that there was no public-law element to the termination of Ms Wedderburn’s employment last December. Respondents in the case welcomed the judgment and the Ministry of Health added that the allegations made by the former BHeC chief executive, who claimed her sacking was politically motivated, were “baseless”. Mr Johnston said: “Ms Wedderburn has faith in Bermuda’s courts. Although she is taking on a government whose pockets seem to have no bottoms, and even though her own finances are strained, she believes that in time, what she said took place at the Bermuda Health Council between 2017 and 2018 will be judged against what the Government says occurred — and the appropriate result will be reached.” The lawyer said Ms Wedderburn hoped a future outcome would “correct” her termination and also make sure that “a governmental body which is so important to every resident’s healthcare on the island operates as the Bermuda Health Council Act 2004 and the general laws of Bermuda demand”. Ms Wedderburn made an application to the Supreme Court for judicial review in March. She alleged that David Burt, the Premier, interfered in the running of the BHeC to push taxpayer-funded payments to Ewart Brown, a former Progressive Labour Party premier. Ms Wedderburn claimed in the proceedings that Kim Wilson, the Minister of Health, and Alicia Stovell-Washington, then the BHeC chairwoman, interfered with the day-to-day operation of the council. She sought to win an order that would quash her termination The allegations were vigorously denied during a one-day hearing in front of Mr Justice Kessaram last month, when lawyers for the parties presented arguments on whether the case involved matters of public law, suitable for a judicial review, or private law, where an alternative legal remedy could be sought. His written judgment was delivered on Wednesday. Mr Johnston explained later: “After Ms Wedderburn was fired as CEO of the Bermuda Health Council on December 7, 2018, she didn’t, at the height of emotion, run to the Supreme Court and make an application for judicial review. She sat, read through documents, and with deliberateness, considered the implications of bringing a case like this against the public officers who are at the centre of the allegations she makes. She knows the allegations are very serious, and she understood, from the start, that the Government would likely use every resource at its disposal to keep those allegations from being tested in any public forum. Six months have passed since Ms Wedderburn started these proceedings, but this case is still in its infancy.” He said that the judgment would be “looked at thoroughly”. Mr Johnston added: “The implications of the ruling will be considered, and whatever steps are deemed most appropriate will be made.” Juliana Snelling, the lawyer for the health council and Dr Stovell-Washington, its former chairwoman, told the court in September that the health council voted eight to one, with no abstentions, to end Ms Wedderburn’s employment on December 6 last year because of dissatisfaction with her leadership. She said Dr Stovell-Washington contacted Ms Wilson after the vote was taken. The next day, the pair spoke again before Ms Wilson e-mailed approval of the decision. Ms Snelling said last week: “The respondents are very pleased with today’s Supreme Court’s judgment, which is consistent with their position all along that the issue of the former CEO’s separation of employment from the council was never amenable to judicial review.” Charles Richardson, who acted for Mr Burt and Ms Wilson in the hearing last month, said then that Ms Wedderburn should have gone to an employment tribunal, rather than seek a judicial review. A Ministry of Health spokeswoman said: “The Ministry of Health is satisfied with this outcome, as the case was baseless. Likewise, the ministry continues to robustly deny the allegations made by the applicant, which, like the claims disproved by the judgment, are baseless.” A spokeswoman for Mr Burt, who has “strongly denied” the allegations, said yesterday: “The Supreme Court of Bermuda has found that the remedy of judicial review was not available in this case. That is a matter of law. Any party aggrieved of a finding of a court in Bermuda is at liberty to consider an appeal. The media is hardly the appropriate forum to try cases.”
2019. October 10. The Bermuda Health Council (“Council”), in collaboration with the Ministry of Health, has started to gather views on the proposed Bermuda Health Plan. The Council remains committed to collaborating with stakeholders and ensuring health system sustainability for everyone. Since the beginning of the health system reform community discussions, the Council has seen an increase in the attendance in-person and online using ZOOM, which is a teleconferencing option provided to the public. Every meeting is open to the public to allow for open discussion on the scope of the proposed health system reforms and to have in-depth conversations on supporting changes that will need to occur to achieve better public health. The topics discussed to date include Early Childhood Health and Pediatrics, Ensuring Maternity Care and Midwifery, the Conversation on the Unified System Transition Roadmap; and the Single Payer/Unified Model Implications. Dr. Ricky Brathwaite, Acting CEO/Director Health Economics, states, “These conversations have been very insightful and extremely helpful as we lay the transitionary pathway for system improvements. It’s truly important to hear from those on the ground that we have gaps in our development programmes for kids, or that our maternity care is underutilized, or the diverse views that are held about profitability in healthcare and the concepts of shared sacrifice. We have to have these tough conversations if we are going to ensure that the chosen system will be successful. One thing that has been made clear from all the discussions recently, is that the public is definitely engaged and determined to contribute to the maintenance of our good health system parts and the improvement of our weak points.” A full slate of topics are scheduled to occur at least three times each week during the upcoming months. After each meeting, there will be information published on the Council’s website giving details from the meetings of the community discussions presented. Those interested in attending in-person are encouraged to RSVP as space is limited. In addition, those who cannot attend a meeting in-person are welcome to find us online using ZOOM. The online teleconference service will allow you to hear the discussion and participate by sending your questions and feedback, live. Ad-hoc meetings for interested stakeholder groups can also be arranged. These requests must be made at least five (5) working days in advance and will be scheduled based on availability. Topics that have been discussed during one of the sessions, but need further depth of discussion, will be automatically added to the schedule.
2019. October 10. The former chief executive of the Bermuda Health Council was told that the organisation’s decision to sack her could not be judged as a matter of public law. Tawanna Wedderburn applied for a judicial review in the Supreme Court, alleging that the termination of her employment last December, was politically motivated. She took action against the health council, its former chairwoman Alicia Stovell-Washington, Kim Wilson, the Minister of Health, and David Burt, the Premier. The allegations were vigorously denied during a one-day hearing last month, when Assistant Justice David Kessaram heard arguments on whether Ms Wedderburn’s case involved matters of public law, suitable for a judicial review, or private law, where an alternative legal remedy could be sought. A written ruling on the preliminary issue was handed down by the judge yesterday. Mr Justice Kessaram said in the judgment: “I am inclined to find that, if what the applicant alleges is true, she would have a compelling case that the council and the minister acted for improper purposes and in bad faith towards her as CEO of the council. But is that enough to give rise to a right of judicial review of the decisions that resulted in her dismissal?” He found that Ms Wedderburn’s “analysis of the facts leading to her firing” did not fit with the Bermuda Health Council Act 2004. Mr Justice Kessaram said the former chief executive’s statement that the council had a duty to “recommend” the health minister that her employment was terminated suggested it was the minister who made the decision. He added: “This does not seem to me to be a correct analysis.” Mr Justice Kessaram wrote: “What is remarkable about the relief claimed is what is not sought. There is no relief sought in the way of damages for wrongful dismissal, or for an order for reinstatement in her position as CEO, or a declaration that her employment continues until properly terminated in accordance with the Act and her contract. Damages are sought, not for compensation for loss arising out of any breach of her contract of employment, but against the Premier, the Minister of Health, the chairman of the council and the council for misfeasance in public office, a tort.” The ruling showed it was agreed that Ms Wedderburn was not a public servant or holder of a public office and that her employment terms were not regulated by statute or regulations. Mr Justice Kessaram wrote, it was argued on her behalf that there was a public law element to her role, in that there was a statutory requirement for the health minister to approve any decision to terminate her contract. He added: “It is said that this fact makes the decision to terminate amenable to judicial review. I do not agree.” The judge noted that he made “no finding as to the lawfulness of the termination” of Ms Wedderburn’s employment. He said: “It may very well be the case that the decision of the council and the decision of the minister were made in bad faith and for improper purposes. Those are issues which, if they are to be decided in these proceedings, can only be decided after hearing the evidence.” Mr Justice Kessaram found there was no public law element to the termination and that it was “not amenable to judicial review”. He said in court yesterday that he expected the parties to “collaborate with each other” about how to proceed in terms of the remaining issues in Ms Wedderburn’s claim and adjourned the matter until a later date.
2019. October 4. Bermuda’s working population can expect to paying out twice as much on healthcare in 20 years as they do today — and that’s if the island’s healthcare costs remain the same. That is the view of Ricky Brathwaite, acting chief executive officer of the Bermuda Health Council, who was speaking about the impact of demographics on the healthcare system. Total annual healthcare spending on the island is about $700 million, or $11,300 per person, Mr Brathwaite said during a panel discussion at the Bermuda Insurance Market Conference, organised by the Bermuda Insurance Institute. “The number of working individuals to every senior is 3.9 — in 20 years that number’s going to shrink to 1.7,” Dr Brathwaite, a health economist, said. “That means that even if we stayed at $700 million, and unless we want seniors to pay more, that 3.9 to 1.7 means a doubling of the cost for those contributing.” The panel, which also featured Michelle Jackson, senior vice-president, group lines health and life at BF&M, and Michael Richmond, chief of staff at the Bermuda Hospitals Board, agreed that the Bermuda healthcare system needs transformational change as it faces pressures from the growing prevalence of chronic diseases and an ageing population. “The burden of the population not growing, but ageing, will fall on you,” Dr Brathwaite added, referring to a relatively youthful audience. “Solutions have to be arrived at now, or you will face the results of non-action. Unless something is done in the next ten to 15 years in transformational ways, you’re going to bear the cost of a system that didn’t adjust to deal with higher levels of chronic conditions. That has a huge effect on productivity and on the economy.” Dr Richmond joined the BHB two years ago, having previously worked in Qatar, where he said the health system’s challenge was dealing with 20,000 more people every month. He expected Bermuda, with its stable population, to be less challenging, but soon discovered the island’s complexities. “The demographics facing Bermuda are simply quite staggering, the growth of chronic disease is staggering, the lack of integration in the health system is staggering, the lack of information is quite staggering, and we have a primary care and community care system which is under enormous pressure,” Dr Richmond said. He added that the pressures on the healthcare system had shifted from infectious to chronic diseases over recent decades. In the US, he said the obesity rate had gone from 11 per cent in 1973 to 70 per cent today. In Bermuda, 75 per cent of people are obese or overweight, according to research cited by the BermudaFirst group. The management of chronic disease should be much more in the domain of primary care than the hospital, Dr Richmond said. “The role of the hospital is when those chronic diseases get out of control,” Dr Richmond said. “Have we reached that point?” asked Kim Wilkerson, the panel moderator, who is head of claims at Axa XL in Bermuda. “We reach it every day,” Dr Richmond replied. Asked about the impact on the hospital of the ageing population, Dr Richmond said an increase in chronic diseases, such as diabetes and dementia, could be expected in an older population. “If nothing were to change, we would need another 70 to 80 inpatient beds at the hospital,” he said. “That’s an enormous cost and it’s also not a very good plan.” Most other jurisdictions facing similar issues had looked to increase community care provision, he added. Ms Jackson said the solutions to the healthcare challenge had to be comprehensive. Blaming particular parties, such as insurers, the Government or physicians, was not the way forward, she said. “The system is multifaceted and we need a multifaceted solution,” Ms Jackson said. “We all have a part to play.” The solution had to encompass technological, educational, social and regulatory components. “You can’t achieve transformational change with one magic bullet,” she said. Ms Jackson defended the health insurance industry against the notion that they took too much out of the system in profits. “All of the health insurers have diversified businesses, so to think that the financial statements of these companies are all about health insurance is missing the point,” she said. “It’s not a high-margin business — quite the opposite. The margins are really slim and if you’re profitable, you’re lucky. To suggest that health insurers are making out like bandits in this environment is way off the mark.” The medical loss ratio of the government health insurance plans was about 140 per cent, she said, meaning that for every dollar in premium, $1.40 was spent on claims. “If the private insurers did that, there would be no private insurance available,” Ms Jackson said. “If you think of the risks and the extreme probability of high catastrophic claims that are absorbed, it’s a very challenging business.” Mr Brathwaite said naturally private insurers were in business to make a profit, but posed the question of whether healthcare should be regarded as a social service, rather than a profit-making business. He added: “There’s only a certain amount of money in healthcare and if some of that money that could be going towards prevention is going on profit, then you have to take a step back and ask: are we benefiting the population in how we allocate the money? So it’s not a question of whether health insurers should make a profit, it’s a question of are we using all the money we have to spend on healthcare in the best way for the people?” Ms Jackson said health insurers contributed through the valuable data they provided to the regulator and through the incentives they provide to clients to live healthier lives, she added. “The health insurance business does better when people are healthier,” Ms Jackson said. “So the insurers on the island spend a lot of time trying to put together packages to try to get people to live healthy lifestyles. It’s simply good business for health insurers in a business where frankly, the demographics are not in our favour.” The BermudaFirst group has proposed a change from the “fee-for-service” approach to an outcome-based system. Dr Brathwaite said: “Are there incentives within physician practices to make money based on the number of services provided? Yes. Are there individuals who may take advantage of the opportunity to do so? Yes. That doesn’t mean that they’re wrong. It means that the system is set up for them to be able to do it.” He said the outcome-based approach needed everyone in the industry to work together and agree to the same set of standards. Ms Jackson said: “The vast majority of physicians on the island are high quality, but there are perverse incentives within the Bermuda healthcare system. There are tremendous conflicts of interest where physicians own additional services — labs, or pharmacies, for example. I think there are some fundamental things there that we have to address to eliminate those conflicts of interest.”
2019. September 28. Bermuda’s health minister was questioned yesterday on whether the Government had misled the public on the scope of public consultation on healthcare reforms. Scott Pearman, the Shadow Minister of Legal Affairs, pointed to a town hall meeting in Sandys this month to discuss the Bermuda Health Plan 2020. Kim Wilson announced in August that the plan was to replace the Standard Health Benefit coverage for all island residents. Mr Pearman said that Ms Wilson had told people at the meeting that the Government had already decided to proceed with the reform and that public consultation was limited to the benefits that would be included in the new plan. He told the House: “Given the expressed statement that you made in Somerset, would you agree it is misleading to suggest to this House that you have begun a consultation on any other ways to ensure affordable healthcare for all?” Ms Wilson responded: “Absolutely not.” She told MPs that the consultation period was twofold. Ms Wilson said that the first part of the period was to “ascertain from the public the nature of the benefits to be included”. She said part two would outline the road map to transition from the current “disjointed, ineffective” plan to the new scheme. Ms Wilson reiterated that a “soft launch” of the new plan was expected next autumn. But Mr Pearman pressed: “If the only scope of the consultation are various permutations of your single option, that is not a full and proper consultation, is it? What would you say to members of the public who don’t want your basic plan at all?” Ms Wilson said that the Government had been elected to provide “for the basic human right of affordable healthcare. And that is exactly what we are going to do.” The exchange came during Question Period after Ms Wilson made a ministerial statement to provide an update on the public consultation process. She said: “We have begun a period of public consultation, during which we are speaking to stakeholders and the public on how we can ensure all of Bermuda’s residents can have affordable access to healthcare.” She told MPs that a “decent package that is affordable and available to all is fundamental”. Ms Wilson added: “To do this, we have to change the way we pay for healthcare.” She said that the Government’s decision to adopt a unified finance model had been made “following extensive considerations”. Michael Dunkley, a One Bermuda Alliance backbencher, questioned what other similar jurisdictions had adopted the unified model, and what if any analysis had been done by the Government to gauge its success elsewhere. He also asked when the cost of the BHP would be firmed up. Ms Wilson pointed to the Bahamas, where she believed the model had been launched “within the last several months”. She added: “I’m not even sure it’s a year old.” Ms Wilson said that the cost would be based on public feedback on what benefits they wanted included. She explained: “The more benefits that are offered, the more expensive the plan. So until we have an opportunity to gauge the public’s sentiment as to what benefits will be included, we can’t cost anything.”
2019. September 17. The Government intends to “soft launch” a significant revision of Bermuda’s healthcare next autumn, but full implementation could take years. Kim Wilson, the Minister of Health, told a town hall in Sandys last night that the details of the Bermuda Health Plan and how it will be rolled out are still under discussion as the consultation process continues. Ms Wilson told an audience of about 50 at St James Church Hall that the Government will work with stakeholders, such as insurers and doctors, to determine how the transition from the existing healthcare model to the new scheme could be carried out. She suggested that it may be decided that a percentage of the population be moved into the new system, with more being added over time. Ms Wilson added: “It may be a couple of years before all 65,000 are in. The stakeholders will be able to say what would be reasonable to expect.” She said the existing standard healthcare benefit offered little in the way of preventive and primary care, which the new plan is intended to address. Ms Wilson said: “With the standard healthcare rate, 95 per cent of it is for inpatient and outpatient care. We are looking at cases where people say they can’t afford to go to the doctor because they can’t afford the copay, so we want to include primary-care visits with a regular fee, a regular copay, to encourage people who are saying they can’t go to a doctor to go for their annual visit.” She said such an approach would mean issues may be caught and addressed sooner, which would reduce overall healthcare costs. But Ms Wilson said the specifics of what the plan would contain, and what it would cost, are still up for discussion. A “mock package” for a single adult shows the present yearly cost of $7,058 potentially dropping to $6,308, with suggested savings such as:
Ms Wilson explained the meetings are intended to gather public feedback about what benefits they want to see, along with what premiums and co-pay are reasonable, to find the right balance. Ms Wilson added the ministry had already been told by some that the $400 coverage for prescription medicines seemed too low, but said the standard healthcare benefit does not include such coverage. The Bermuda Medical Doctors Association voiced reservations about the plan on Sunday and complained about the level of consultation with doctors. Ms Wilson responded yesterday that the ministry was “fully committed” to continued dialogue with physicians and healthcare providers. She said: “The Bermuda Medical Doctors Association statement reflects both the shared interest in putting patients first, and the mutual desire to continue dialogue. The ministry has been made aware of the BMDA’s position with respect to the Government’s decision to adopt a unified model of health financing. Their concerns are important and will inform the consultation and development of a transition road map to phase reforms gradually and avoid unintended consequences.” Ms Wilson added that a BMDA representative was included in the Health Financing Reform Stakeholder Consultation Group last year and BMDA members were invited to participate in a survey.
2019. September 12. A re-modeled healthcare system focused on outcomes, an independent education authority, moves to lower the cost of living and immigration policies to address the island’s talent gap are among the proposals in an advisory group’s plan for Bermuda’s future. BermudaFirst revealed Future State Report, the second phase of its national socio-economic plan, in a press conference at the Bermuda Underwater Exploration Institute today. The group claims in the report, which was commissioned by David Burt, the Premier, that the priorities it identified “will enhance the lives of Bermudians and provide citizens with the tools and opportunity to realise their full potential”. The report points out shortfalls, particularly in the island’s education and healthcare systems, and spells out recommendations to address them. It also challenges Bermudians to show the courage in leadership and willingness to change that is necessary to meet the challenges the island faces. “If we are going to change Bermuda’s trajectory, we will have to change our mindsets to deal with the social and economic realities of the 21st century: a shrinking and ageing population, an under performing education system and healthcare costs that are spiraling out of control,” BermudaFirst states. BermudaFirst’s roots in lie in a think tank led by reinsurance veteran Don Kramer, comprising business and political leaders and formed in 2009 with the aim of finding solutions to the island’s economic challenges. The group was resurrected by the Bermuda Government in 2017, this time including no politicians and led by chairman Philip Butterfield, the former chief executive officer of HSBC Bank Bermuda. Other members represent sectors including business, charities, unions and education. The report identifies four global trends impacting life in Bermuda: rising inequalities, the rapid rate of technological change, tribalism and climate change. Action on education, healthcare and talent/immigration are seen as “critical priorities”. BermudaFirst points out the underperformance of the public education system and that consequently “one glaring reality is the portion of our population that is unable to compete for existing job opportunities, much less present themselves as candidates for emerging 21st century work! If we fail to act decisively now, our passivity will be viewed as the most significant missed opportunity in the history of the island.” It adds that the public education system “lacks accountability at all levels” and calls for an independent authority responsible for performance management of educators and a requirement that all teachers be internationally certified by an approved list of institutions. The group envisions a “world-class public education system that produces student outcomes where our children can successfully compete in the global marketplace”. In healthcare, the report cites research showing that nearly 10 per cent of Bermudians have no healthcare insurance and that Bermudians who have jobs and health insurance spend 18 per cent of their income on healthcare. “The current health system is not sustainable from the perspective of cost, service provision or capacity,” the report states. The report calls for changes leading to a patient-centric, outcome-based billing model focused on value rather than price, and including regulation of healthcare providers. “Bermuda’s model of healthcare must evolve to focus more on outcomes and value and less on the perverse incentives tied to a system that revolves around reimbursement of service,” the report states. “Any model that simply pays without due consideration of actual results leads to excessive utilization at an ever-escalating price.” It calls for a national health education programme aimed at encouraging people to eat better and exercise more, to combat preventable, lifestyle-based diseases that generate a large portion of healthcare costs. Among its recommendations, BermudaFirst calls for reform of the Standard Health Benefit, the basis of how health insurance premiums are set. “Instead of SHB solely depending on a fee-for-service model, create a pooling system that aligns residents to insurance packages based on their income,” the report proposes. “This model will require Government to regulate fees and insurers to establish set rates.” SHB pricing should also be published, it adds. BermudaFirst believes its proposals would reduce healthcare expenditure by 10 to 15 per cent and result in a healthier population. BermudaFirst touches on the impact of demographic trends and projections that show the workforce will shrink as the non-working-age population grows. The report states: “It is also important to note that, if we fix the healthcare industry, but do not expand our population, Bermuda will continue to be challenged with higher than acceptable costs as there will simply not be the number of individuals across which to spread those costs.”
2019. September 11. The chairwoman of the Bermuda Health Council has resigned for “family and personal professional reasons”. Alicia Stovell-Washington said that she had to return to her profession full time after the death of her colleague, the eye surgeon Leonard Teye-Botchway. Dr Stovell-Washington was appointed chairwoman of the health council in October 2017. Her resignation comes four months after former chief executive Tawanna Wedderburn alleged in a court case that Dr Stovell-Washington interfered with the day-to-day operation of the council, along with David Burt, the Premier, and Kim Wilson, the Minister of Health, to push taxpayer-funded payments, to Ewart Brown, the former premier. Ms Wedderburn made the claims in May as part of an application for judicial review before the Supreme Court as part of her attempt to quash her termination as CEO last December. She said that the trio’s interference was unlawful “because it was done for the purpose of controlling the council’s policy decisions, and/or facilitating government payments and/or other pecuniary awards to specific Progressive Labour Party supporters, a former premier, at least one Cabinet minister, and/or others”. A Ministry of Health spokeswoman previously said that the respondents in the case vigorously deny the allegations and are robustly defending themselves in the proceedings, which continued in the courts yesterday. Dr Stovell-Washington said in a statement released by the Ministry of Health yesterday: “I’m very sad to be stepping down from such a vital organisation as the health council, but my personal circumstances require my full attention elsewhere at this time. I must return to my family and my medical practice and advocate for patient care and my own family’s health. Following the recent passing of my colleague, Dr Teye-Botchway, my time and attention must be dedicated to assisting with patient care and continuity in every way I can.” She added: “I am a physician first and foremost, and I must return to my profession full time right now. However, I will continue to support the health council and the Ministry of Health in every way I can, particularly at this time of important reforms and a transformation of our health system.” Ms Wilson said that she was saddened to accept the voluntary resignation. She said: “It is absolutely evident that the health council grew and evolved during Dr Stovell-Washington’s chairmanship and I’m entirely indebted to her for her dedication, fortitude and immense contribution. I know that she leaves the health council stronger than when she took over. While I am saddened at the reasons for her need to step down at this time, I’m confident that Dr Stovell-Washington will remain a stalwart of fairness in the health system and will continue to be an advocate and partner in our efforts to make Bermuda healthier.” The ministry’s statement said that Dr Stovell-Washington had “excelled in her leadership of the board and council”. It said: “Under her tenure, the health council refocused its strategic direction, increased oversight and regulation of health insurers, continued to improve its healthcare data repository and dissemination, ensured decisions were data-driven and evidence based, enhanced board governance and grew its relationship with local and international partners such as the Pan American Health Organisation.” Dr Stovell-Washington steps down formally tomorrow. A new chairman will be announced in due course.
2019. September 10. A veteran nurse with almost 50 years on the healthcare frontline is shocked to find she has no insurance coverage for emergency bone cancer treatment overseas. Eloise Bell, 73, said yesterday: “I’ve worked here for 50 years, paid my insurance for 50 years, and the one time I need it I can’t get any coverage.” Ms Bell said she was told by a pharmacist when she picked up prescriptions for blood pressure treatment and painkillers six weeks ago that her health insurance covered only hospital care at the King Edward VII Memorial Hospital. She added: “I couldn’t believe it. I don’t even get a discount for being over 65.” Ms Bell, who had bone cancer in her right leg diagnosed three weeks ago, said she had no choice but to travel to Brigham and Women’s Hospital in Boston tomorrow for further treatment. She added: “If I could get it checked here, I could understand why they won’t cover me overseas. But they won’t do it here. Ms Bell asked: “So what happens to someone who has a condition they can’t handle here? Do they have to die because they don’t have insurance for overseas?” Ms Bell said she now has to find thousands of dollars for her flight, hotel accommodation and treatment in Boston, and did not know what further treatment might cost. She added: “They are causing me to put my life over money and I have 24 hours to make a decision.” Now she has launched an appeal for financial help and obtained a temporary fundraising licence. She said: “This is my appeal to the public to lend their voice in my support. “Perhaps some of the people I have helped over the years will be able to help me out.” Ms Bell said she had cared for thousands of patients over her career, including hundreds flown overseas by the Bermuda Air Medivac plane from 2004 to 2011. Ms Bell was the service’s vice-president and chief flight nurse for the service until it folded. She said her health problem started in April with an ache that she at first thought was a pulled muscle. Doctors suggested arthritis, then myositis, a muscle inflammation, but a CT scan, followed by an MRI, revealed a tumor on her right thigh bone near her hip. Ms Bell said: “You can see on the scan that it is almost through to the marrow of the bone. That’s why there is such time pressure.” She added: “It’s serious. I was told the worst-case scenario is I’ll lose my leg. I had a little cry and then pulled myself together for the next step.” She said a biopsy at Brigham and Women’s would determine if the cancer was malignant or benign. Ms Bell explained the procedure was said to be “too dangerous to do in Bermuda”. She added: “In my 50 years as a nurse, I have had one inpatient hospital visit, for the delivery of my daughter. I have been off ill about ten days.” Ms Bell retired from the hospital seven years ago, but she has been employed there ever since in full-time, part-time and casual roles. Ms Bell explained that casual nurses were called in when the hospital was short staffed, and were “not supposed to work more than a certain number of hours per year”. She added: “All I knew was I had hospital insurance. I didn’t think it mattered whether it was Bermuda or Timbuktu.” Ms Bell said a part-time nurse from overseas had a massive heart attack last year while he awaited a new contract. She added: “He had no insurance because he hadn’t started his new contract. He told me he thought he would have a second heart attack when he found out it cost about $100,000, but they still covered him. I never knew my insurance only covered me for hospital here. I don’t have FutureCare because I don’t need it. Last month, I did full-time hours in the emergency room, so I should be covered for that.” A spokeswoman for the Bermuda Hospitals Board confirmed last night that Ms Bell was “a casual at BHB”, but said that board could not comment on individual cases because of employment confidentiality. She added: “However, we can confirm as a matter of policy, all staff are offered the BHB retiree health plan when they retire from BHB, which includes overseas care as part of major medical. People who do not take up the plan due to their pursuit of alternate employment or their decision to take a health plan independently, forfeit their option to join the retiree plan. Those who take alternate employment post retirement, including working at BHB as a casual, are subject to the health plan offered by the employment. BHB casual health benefits only cover those required by the Health Insurance Act.”
2019. September 4. The chief executive of the Bermuda Hospitals Board is to retire next year after 40 years in healthcare. Venetta Symonds, 61, is to stand down at the end of July after she handed in her notice two weeks ago. Ms Symonds said: “My contract says I have to give six months’ notice. I gave a year’s notice, so the board can work together, along with the health minister, and figure out the next phase. It takes a long time to determine who you need and what the process will be, going forward.” Ms Symonds said most people in a similar role spend two or three years in the job, and that she will have done eight years by the time she retires. She became CEO in 2012 after six years in the deputy CEO role, which included an eight-month stint as acting CEO in 2006. Ms Symonds had a baptism of fire as acting CEO, after she found herself in the middle of a row over plans to build the new hospital on part of the nearby Botanical Gardens. She had to face down hundreds of angry people at town hall meetings, organised to discuss the proposal. Ms Symonds said: “I stood there, looking at this crowd and trying to understand their passion, and trying to rationalize it, against the reality of putting things on a green field. The lesson I walked out of there with was, you have to listen. You can’t make a decision that is huge, without engaging and bringing the public along with you.” The BHB backed down and changed their plans. Ms Symonds said: “When it went for the final permission at planning, when there could have been a thousand signatures saying ‘no’, no one registered a concern.” Ms Symonds started at the King Edward VII Memorial Hospital as a 17-year-old summer student and worked as a file clerk in the radiology department. She became interested in radiology and won a BHB scholarship to get an associates degree in the subject. The scholarship was only for two years, but, when she passed her board examinations with flying colours, she decided to study for a bachelor’s degree. However, the scholarship committee said she was already qualified, and wanted her to start work right away. One committee member told her: “What do you think you’re going to do? Come back and be CEO?’.” The committee gave in and paid for an extra two years at the University of Tennessee in Memphis, and she returned to start work as a certified radiology technologist in 1980. Ms Symonds said: “I was so nervous and scared on my first day. People laugh at me when I say I am shy, but that day, I kept my head down, even when going into the cafeteria. I felt like there were all these people looking at me.” She was promoted to manager in the radiology department in 1998, after Adrian Ringer, then the head of the department, said if she could keep hospital administrators off his back, the job was hers. The post of chief operational officer came up around the same time, and the BHB chairman visited her at work and said she should apply for the job. Ms Symonds said: “The reason I am here is because different individuals have spotted something in me, and they encouraged me. When I was nervous and didn’t have confidence, they had confidence. I have had an incredible journey, to get here.” She added she was grateful to her parents, Norris and Ilis Pearman, for their support. Ms Symonds said: “Towards the end of her life, my mother would sit there, and say, ‘I can’t believe you are CEO of the hospital’. The tears would come. I said ‘mummy, okay, it’s been five years’. She’d say ‘but I can’t believe it’.” Ms Symonds said medical technology had changed since she started as a radiologist, when she would have to wet develop X-ray films, a process that is now digital. She added she had seen the first MRI scanner arrive at the hospital in 2002. “The machine came in a pre-made building. They had to lift the building off the ship and onto the dock. It was put on a trailer and we all walked behind it, to the hospital. They had to change the medians in the road to accommodate us.” Ms Symonds said she planned to explore a new-found passion for art, gardening and travel, as well as spend more time with husband Carlos and adult children Marcus and Natasia. William Madeiros, the BHB chairman, said: “BHB has flourished under Ms Symonds’s vision and direction. Quality has improved, there is a strong strategy in place driving exceptional care, a strong partnership and a healthy community, and BHB has become a more open, transparent and caring partner under her leadership.”
2019. August 15. Proposed reforms to health benefits should not be examined to a tight deadline, an insurance industry leader warned. Peter Lozier, the executive vice-president of group insurance at Argus Group, said that “health reform of this magnitude and complexity requires comprehensive input from a breadth of stakeholders”. He added: “As many details are yet to be determined, we encourage the adoption of a flexible, rather than fixed, consultation period to ensure all stakeholders have the opportunity to be heard.” Mr Lozier was speaking after plans were unveiled last week for a revised package of health insurance benefits designed to cut out-of-pocket expenses for the public. Kim Wilson, the Minister of Health, said that the Bermuda Health Plan 2020 would replace the Standard Health Benefit coverage for all the island’s 65,000 residents. But the level of coverage, as well as who will administer the scheme, remain unclear. Ms Wilson said that consultation documents on the plan would be released “over the coming weeks” and that there would be a four-month consultation period on what the plan should include and cost. Responsibility for administration of the plan will also be discussed. Mr Lozier said that the company had a responsibility to help lower healthcare costs on the island. He added: “We support solutions that better balance affordability and quality care. We remain an active contributor in the Health Financing Reform Stakeholder Consultation Group and welcome further consultation by the Government as they develop the Bermuda Health Plan.” Mr Lozier said that healthy lifestyles, backed by healthcare professionals, “is the key to driving down overall health costs. This is why Argus continues to invest in chronic disease prevention and care management to improve the financial and physical wellness of Bermuda residents. We are committed to working with the Government to provide health management tools and programmes that improve the population’s health.” Naz Farrow, the chief executive of insurance firm Colonial Group International, said last week that the company agreed with the “high-level goals” proposed in the BHP. But she warned: “The proposed creation of a ‘new healthcare system’ will be a massive and complex undertaking requiring the highest degree of technical and financial planning, co-ordination and community co-operation.” Ms Farrow said the company welcomed Ms Wilson’s “commitment to meaningful and effective consultation with stakeholders”. She added: “We also appreciate the minister’s statement that the road map to achieving the 2020 plan, as she framed it, is ‘complicated’ with much to be made clear on economic, administrative and transitional questions that will have material effect on the viability of the plan itself.” Insurance firm BF&M did not respond to a request for comment. Ms Wilson said last week that the unified system was “best suited to achieve efficiencies, economies of scale and cost savings. A unified system means that all residents will be in the same basic insurance pool, sharing health costs throughout all of Bermuda’s residents.” The government website estimated the prospective plan could cut health expenditure for a family of four from $25,536 a year to $17,068 compared to the present system. A hypothetical model for a single adult showed the annual cost of $7,058 going down to $6,308, with suggested savings such as:
2019. August 12. Bermuda’s health watchdog has started the search for its next chief executive. The Bermuda Health Council has invited applications for consideration for the role of chief executive. And the regulatory body is also on the hunt for a health economist. Ricky Brathwaite has served as acting chief executive since December. He joined BHeC as programme manager for health economics in 2014 and later became director of health economics. Dr Brathwaite was made acting CEO of the regulatory body after former chief executive Tawanna Wedderburn was fired. He did not respond to questions about the job postings by press time yesterday. Advertisements of the posts were published last week. The council said that the role of chief executive was appointed by the BHeC board and reports to the board through the chairman. It added: “The CEO recommends and participates in the formation and revision of policies and programmes by the council and is responsible for implementing and directing, through effective leadership of staff and operational supports, the policies and programmes approved by the board, in accordance with the council’s strategic goals as determined by the board. The CEO is responsible for the successful management of the organisation to meet the goals and objectives as set out by the board.” The successful applicant will, among other responsibilities, be required to oversee day-to-day operations, communicate with the health ministry as well as other community and stakeholder groups, and lead the recruitment, hiring, training and termination of staff. The person will hold a master’s degree in the healthcare or management field, as well as a minimum of ten years’ post-qualification experience in a manager or director’s post. Business and management experience, experience with the development of public health policy, and experience with a regulatory organisation are considered assets. The health economist “provides advisement and guidance ... on health system costs, opportunities for efficiency, implications of system change, and the forecast of demand within the healthcare system”. The job description adds: “The health economist collaborates with local and international partners on research in the areas of health economics, profits and loss, insurance market dynamics and consumer preferences — working towards a more affordable health system that will produce more healthy lives to help grow Bermuda’s economy.” The successful applicant will be responsible to develop and implement strategies, develop and execute projects and programmes, and monitor the status of programmes. The successful candidate will hold a postgraduate degree in economics, finance or a field related to health economics and a minimum of seven years of post-qualification experience in the health system. Ms Wedderburn revealed in March that she would take legal action over her termination which ended an 11-year career with BHeC. Ms Wedderburn said that she had asked for judicial review proceedings against David Burt, the Premier, Kim Wilson, the Minister of Health, her former employers and Alicia Stovell-Washington, the chairwoman of the council. The health council was set up to regulate private health service providers, ensure the provision of essential health services and to promote good health. The BHeC told The Royal Gazette its policy is not to respond or discuss HR matters or personnel issues.
2019. August 10. Plans for a broader, cheaper standard health coverage package to encompass all the island’s residents were given a cautious welcome yesterday. Charles Jeffers, the deputy chairman of the seniors advocates Age Concern, called a proposal to revamp the Standard Health Benefit “long overdue”. Mr Jeffers said: “Age Concern has pushed for this for years. We need to get basic benefits under one banner and away from insurance companies dealing with the extras. If we don’t, there’s nothing to stop insurance rates continuing to go up. They are in the business of making money and satisfying their shareholders. If we have our basic benefits under one set of administrators, we stand to benefit. We are looking at this proposal closely, because a lot of pensions are being taken up with health insurance. We’re hoping the Government is prepared to do whatever is necessary to bring down costs.” The present coverage of the Standard Health Benefit has limited cover for doctors’ visits, prescription drugs or dental care. The revised benefits, tentatively planned to begin late in 2020, are anticipated to bring savings by combining residents in a single unified pool. However, a veteran industry insider, requesting not to be identified, predicted “heavy jobs losses” for the health insurance industry. He said: “A universal health programme means insurance benefits being taken over by the Government and taken out of the hands of private insurers. We are not the first country to do it — Bermuda is late to the universal health insurance game. But everything comes with pros and cons. Hopefully, it leads to coverage for everybody from the womb to the tomb. But the bad thing about universal insurance is it causes queues. Emergency care is pushed up the line. If you’re waiting on knee surgery, you can be pushed down the line. This is a known fact — it’s happened in every area where universal insurance has been implemented.” He questioned how it would be paid for: “Countries with universal health insurance have high taxes. All these things have to be factored in.” Mark Selley, the chairman of the Bermuda Healthcare Advocacy Group, was skeptical. He said the planned four-month consultation period was “not giving us enough time”. He added: “There’s no doubt that healthcare needs to be fixed, but I don’t think this is going to work the way the Ministry of Health is planning. Will this be a huge loss for the private insurers? The co-pay is not legislated at the moment. Will there be an uproar from doctors if the Government puts that control in place? There’s a lot of questions about this. We have not received any prior warning. Until we’re told more about how they intend to move this forward, we don’t have any idea how it will work.”
2019. August 9. A revised package of health benefits could cut out-of-pocket expenses for the public, according to plans unveiled by Bermuda’s health minister yesterday. However, specifics on what the new plan will provide, as well as who will administer the scheme, remain unclear. Kim Wilson said that the Bermuda Health Plan 2020 would replace the Standard Health Benefit coverage for all the island’s 65,000 residents. She said that the proposed unified system “is best suited to achieve efficiencies, economies of scale and cost savings”. The minister told a press conference: “A unified system means that all residents will be in the same basic insurance pool, sharing health costs throughout all of Bermuda’s residents.” The government website estimates the prospective plan could chop annual expenses for a family of four from $25,536 to $17,068 compared with the current system. A hypothetical model for a single adult shows the present yearly cost of $7,058 potentially dropping to $6,308, with suggested savings such as:
Naz Farrow, the chief executive of Colonial Group International said yesterday that the company supported a scheme to improve health and reduce costs, but warned the creation of a new system was a “massive and complex undertaking”. Ms Wilson said that the new benefits package “will be designed to help make us healthier and result in real savings by placing caps on co-payments while ensuring healthcare businesses can be financially stable”. She added that a new draft plan for public consultation includes “access to doctors and specialists, home-care services and basic coverage for medicines, dental, vision and overseas care”. Ms Wilson said that it was estimated the BHP could be provided for $514 a month for adults and $178 a month for children. She added: “This would be $257 each, when shared between employer and employee. It would replace SHB and, therefore, includes everything already in SHB.” Responsibility for administering the plan had yet to be decided, she said. It would be part of a twofold consultation expected to last four months. Ms Wilson explained: “One, it will be to decide what does that Bermuda Health Plan 2020 look like — what type of benefits should be included. The second part of the consultation will include the development of a road map as to how we will effectively transition our health financing from the current, disjointed, expensive methodology towards a unified system.” Ms Wilson did not rule out a possible quango arrangement to administer the plan, in addition to private and government-run schemes. She was tight-lipped on whether one administration model was preferred over another. Ms Wilson said: “The consultation period will allow members of the public and private sector to participate in this process. It is very important that they are fully engaged. No decisions are final.” Ms Wilson said that health insurance providers had been “intimately involved” with consultation to date. She said that a stakeholder consultation document that detailed feedback from health insurance providers and other groups would be available in “due course”. Ms Wilson issued a “caution” to Bermudians in her speech. She said: “There will be members of our community who will be content with the status quo, not wishing to advance the reform measures I have just spoken about, and who think that the fundamentals of our healthcare system in place for the last 50 years should continue. This government does not agree.” Ms Wilson did not provide an answer when pressed on what specifically would be opposed in the new plan, She said: “I can anticipate, without looking in a crystal ball, that if we change a system that has systemically disserviced a large segment of our population for over 50 years, that there are likely going to be detractors.” Ms Farrow said that Colonial agreed with the “high-level goals” proposed in the BHP. She added: “The proposed creation of a ‘new healthcare system’ will be a massive and complex undertaking requiring the highest degree of technical and financial planning, co-ordination and community co-operation.” Ms Farrow said the company welcomed Ms Wilson’s “commitment to meaningful and effective consultation with stakeholders”. She added: “We also appreciate the minister’s statement that the road map to achieving the 2020 plan, as she framed it, is ‘complicated’ with much to be made clear on economic, administrative and transitional questions that will have material effect on the viability of the plan itself.” John Wight, the president and chief executive of BF&M, said the company had no comment for now. Questions sent to insurers Argus Group were unanswered by press time yesterday. However, Patricia Gordon-Pamplin, the Shadow Minister of Health, called the announcement a “flavour of the month”. She said the plan was a move by Ms Wilson “to show their relevance and to attempt to dupe the public that something is being done to control costs” and that it came amid “a total lack of transparency concerning the vision for healthcare and curtailed costs”. Ms Gordon-Pamplin added: “In the past parliamentary year, the minister has announced and passed legislation to effect several piecemeal changes to the healthcare system, which has resulted in increased health insurance costs as there is a clear lack of understanding of the drivers of healthcare costs.”
2019. August 7. The Bermuda Health Council has asked people for “innovative solutions” to help fight against serious diseases. The Council is developing a Chronic Disease Innovation Programme, which will fund initiatives to address high rates of non-communicable chronic diseases and associated disabilities. It has launched an online survey to get suggestions from the public. Tiara Carlington, the project manager, said: “In some way, we are all impacted by the growing burden of chronic disease in Bermuda, whether as patients, friends, family members, employers, health insurers or health providers. However, we are not of the belief that the status quo is the only pathway to the future. We imagine that through a collaborative approach we can do much better and enable better health for all. This fund creates an opportunity for the system to explore new ways of reducing the burden and improving the health of the population.” A BHC spokeswoman said: “Health professionals, community leaders and groups know what is needed to support and strengthen the health of the population. Given this existing knowledge, there are valuable resources within the community that are in an ideal position to propose interventions that align with Bermuda’s national strategies for improving public health.” The spokesman said that all members of the public can submit ideas for health interventions. The BHC will then put out invitations for formal proposals. Funding for the programmes will be based on the evidence which supports the proposal, the scale of impact, the projected and supported return on investment and sustainability of the benefit. Initiatives will also be considered based on their ability to address risk factors that are common across chronic conditions, such as smoking and obesity. The spokeswoman added the initiative is funded through insurance, with a portion of this year’s Standard Premium insurance rate going towards the programme. She said: “All funds will be used to support public health interventions that consider local context, are derived within the local environment, and can complement the health system in addressing this major health system issue of chronic disease. The BHC will provide programme oversight, and all reporting of the use of awarded funds and outcomes resulting from the funded initiatives will be made public.” Ricky Brathwaite, the acting CEO, said there has been a deliberate shift of focus to find ways to prevent and manage chronic diseases in Bermuda. Dr Brathwaite said: “We are thinking about long-term investments in our communities and expecting improvements in health and cost reductions. Over time, there have been some really great ideas that have been brought forth by members of the public, and we are excited that we now have an opportunity to empower our communities.”
2019. July 24. Bermuda Hospitals Charitable Foundation (BHCF) today announces a third $350,000 donation to the Bermuda Hospitals Board (BHB) in three years for scholarships and employee training taking the total donated to over $1 million. This third donation was made jointly with the Bermuda Wellness Foundation (BWF). The three donations have funded 28 scholarships since 2017 for students pursing degrees in nursing, physical therapy, occupational therapy and other healthcare related occupations. as the donations have also been used to offer new scholarships including the Dashunte Burgess Nursing Scholarship for students training in nursing at the Bermuda College and Mental Health Nursing scholarships. Upon graduation and completion of their board exams the recipients of the scholarships will be the first Bermudians to be trained in mental health nursing in over 25 years. The donations used for training have given employees the opportunity to pursue courses in wide range of disciplines: 14 members of the BHB’s talent pool (high potential future leaders) recently achieved their Level 5 Certificate in Leadership & Management from the Institute of Leadership Management, a physician was sponsored to pursue studies at the Institute for Healthcare Improvement, and staff benefited from training in a number of specialized areas including information system management, human resources management, developmental learning, occupational health, speech therapy, food services, and nursing. Lisa Sheppard, Executive Director of the BHCF Foundation comments: “Our donors want to see funds make a difference to healthcare in Bermuda. For this reason, we are very pleased to be supporting the Island’s future healthcare professionals knowing that this is an area of great need that will be critical in the long term sustainability of our local services. The training for current BHB employees is making a difference today, supporting clinicians and future leaders at BHB.” BWF Chairman, Jerry de St. Paer says, “The BWF is pleased to join the BHCF Foundation in providing this significant donation to further enhance these critical training resources. Our joint donations also signify a new direction for our organization. The BWF previously acted as a U.S fundraising charity often coordinating our programs and support with the BHCF. As we evaluated future programs and donor initiatives, the BWF and the BHCF have agreed to join efforts under the BHCF and a single Board. We are excited to come together to maximize the support provided to the hospital and to the citizens of Bermuda. We look forward to sharing more information in the coming months.” Scott Pearman, Chief Operating Officer for BHB, adds: “We very much appreciate this and the previous years’ donations from the BHCF and BWF donors. This generosity is helping young Bermudians with their education costs including funding for the first time for much needed mental health nurses. The money is also improving the skills and abilities of our existing staff by funding their training. The most important factor for delivering quality care is people and this donation is an investment in today and tomorrow’s healthcare providers and leaders.”
2019. July 16. Legislation to amend the Health Insurance Act 1970 was approved at the weekend. The change will allow the health minister to make any additional benefit “subject to criteria, including means test criteria, and authorize the Health Insurance Committee to determine the criteria”. Kim Wilson, the Minister of Health, said that amendment will allow the ministry “to continue to provide all persons in Bermuda access to health insurance by ensuring the plans we provide are affordable, focus on quality and ensure access to benefits”. She said the Act will allow for the Health Insurance Committee to provide additional benefits outside of the legislated requirements of the plans, including the home-care benefit. The benefit allows for payment to people caring for elderly and disabled people in their homes. Ms Wilson said that the ministry had to ensure that additional benefits are available to the people most in need. She added that the amendment “provides for the establishment of some criteria for these additional benefits that would include means testing”. Ms Wilson said: “The HIC would also be authorized to determine what the criteria will be for these benefits.” The Health Insurance Amendment (No 2) Act 2019 was passed by MPs in the House of Assembly on Friday. It amends the additional benefits orders made under sections 13(2) and 13B (2) of the Act in respect of the Health Insurance Plan and the FutureCare plan. Ms Wilson said that means testing will only apply to policyholders who apply for HIP and FC after the start of the means-testing provision near the end of the month. She added that 341 people used the home-care benefit at a cost of about $6 million a year. Ms Wilson said: “We want to ensure the viability and sustainability of these plans. To do so is to ensure that the population that needs them the most have access to them. “We cannot do that without establishing some criteria and ensuring there is a process for persons to show they are eligible.” Ms Wilson added the legal change allows the HIC “the ability to do just that”. She said the amendment also reduces the amount reimbursed from HIP and FC for services by overseas providers outside of the Health Insurance Department’s preferred networks. Ms Wilson added that the reimbursement rate would remain untouched for providers inside the network. Jeanne Atherden, a One Bermuda Alliance backbencher, said that it was important to consider those who would be most affected by the change. She explained: “The people who first started to use HIP and FC were those who couldn’t afford private plans.” Ms Atherden added: “Changes today ... are going to affect some of the people that, at this point in time, we really wouldn’t want to affect.” She questioned what the Government was doing to reduce costs. Ms Atherden said: “I don’t see enough to indicate where we are in terms of reducing the utilization. I don’t see enough to indicate where we are with educating people on the role that they play in healthcare.” Michael Dunkley, another OBA backbencher, compared the amendment to “putting a half-inch Johnson Band-Aid on stab wounds”. He added: “It’s not even going to last in the time we put it on.”
2019. June 28. Bermuda’s healthcare system will “implode” if general practitioners have restrictions placed on fees, a doctor warned last night. The source said Bermuda’s GPs faced costs up to three times those of the United States but fought to keep medical costs lower. The doctor said: “If they try to make Bermuda like the National Health Service in Britain, it’s just not going to work. No one will want to work here under that system.” The source added: “The whole medical system here would implode. I would go bankrupt; people would just up and leave.” The doctor was speaking after a marathon 3½-hour emergency meeting held by the Bermuda Medical Doctors Association on Wednesday night. The meeting heard concerns that GPs were being subjected to “heavy-handed” regulations by the BHeC. The source said GPs were ready to protest — and reserved the option to go on strike. The doctor said: “Hospital doctors are not allowed to strike, but community doctors can. We will wait and see what happens, but that’s a possibility. If we stand together, we could form our own union quickly and down tools.” However, he added: “Obviously, no one wants to do that.” Another doctor said: “There are no firm numbers on the table. There’s a lot of unanswered questions and rumblings going back and forth.” The doctor added: “One of the major concerns is what the council would like is to decrease the amount we get, to drive down the cost of healthcare. There is no meeting around the table beforehand. It’s like the Bermuda Health Council is throwing mud at the wall to see what will stick.” The GP said overall expenditure for doctors had been “pretty stable” and was much lower than what was spent on hospital care. The source estimated that about 50 doctors had attended the meeting. Both doctors, who asked not to be named, said they feared Bermuda was moving from public and private funded care to a one-tier healthcare system. Both added there was a widespread belief in the profession that the goal was to “create a system that’s going to decrease our income”. One said: “I believe what they’re trying to do is create a single-tier healthcare system.” However, Ricky Brathwaite, the acting chief executive of BHeC, said: “We won’t expect the physicians of Bermuda to provide a service that can’t pay their bills”. Dr Brathwaite added: “While I appreciate the opportunity to provide play-by-play on these consultation meetings, I think it would be most fair for the process and every person involved to allow these conversations to naturally progress. We are looking forward to having regular meetings with the physician community to talk about healthcare and we will purposefully and meaningfully have them. We expect these to be serious meetings of respect and trust. We expect that any negotiations that take place do not take place in the media, but are done with the patient in mind and with the perspective that we are all in this together. The primary purpose of these meetings is to break down what is working well now in our health system and what is not working well and come up with solutions. We are at our wit’s end hearing about our seniors whose coverage for their prescription meds are done in November and they have to figure out what to do next. Having a 92-year-old have to call around to family members to line up who is going to cover what month of her drugs is just not right. We can’t continue to sell the public of Bermuda a product they cannot afford.” He said the model for Bermuda’s healthcare was “yet to be determined”. He added: “But that is the whole purpose of dialogue. As part of that dialogue, fundamentally we all have to answer the question as to whether everyone deserves the right to have access to health, and if we believe they do, whether everyone is willing to contribute what they can to make that possible.” A spokeswoman for the Ministry of Health said the ministry and the BHeC were involved in “meaningful dialogue” with doctors and other interested parties. She said it was “disingenuous to present discussions as if any decisions had been made”. The spokeswoman added: “The meeting hosted by BMDA was part of constructive dialogue and the process of collaboration will continue. This reaction from one or two physicians is unfortunate and misleading. We look forward to the next level of the conversation with the wider community.”
2019. June 27. A doctor has dismissed the idea that general practitioners were considering strike action. The doctor, who asked not to be named, said that the possibility of job action “was not mentioned at all” at a closed-door meeting held at King Edward VII Memorial Hospital last night. She added: “I would be very, very surprised if it ever was.” However, two physicians, who requested not to be identified, earlier suggested that GPs were ready to protest against “heavy-handed tactics” by the Bermuda Health Council. The doctor said that about 30 to 40 doctors had turned out for the meeting. She said that Ricky Brathwaite, the acting chief executive of the BHeC and its director of health economics, made a presentation to attendees about different healthcare remuneration models. The doctor added: “This is just the start of the conversation.” She said that Dr Brathwaite’s presentation was at first received well by attendees. But she added: “It’s getting a little heated now.” The doctor said that the current relationship between doctors and the BHeC was “better than it has been”. But she added: “We live in worrying times. We all understand that things are getting difficult as the number of insured adults falls. There’s just not going to be enough money to look after people. We are going to need to change the way we deliver healthcare.” The doctor said that island GPs were being “squeezed” by the cost of doing business. She added: “It’s no different than any other people living in Bermuda. It’s uncertain and worrying.” Sources earlier said that GPs were ready to “go on strike” over restrictions imposed by the BHeC. In particular, doctors were described as being “up in arms” over a proposal by the independent monitoring group for doctor’s visits to provide end-of-life care to be capped at $20 per month per patient under the Standard Health Benefit. The proposal was revealed at a meeting last week, it is understood, although sources said that nothing official had been shared with physicians. That move was “the final straw” in the council’s “unilateral” approach to regulating healthcare, one source said. The source added: “This is just an example of how they do things. We will stand together on this; we are not going to take it — if needs be, we will go on a general strike.” But the doctor said that the topic had not been raised at the meeting. She said: “We didn’t even talk about end-of-life care.” Dr Brathwaite, in a statement sent before last night’s meeting, said that it would be “inaccurate and lacking context” to say that the BHeC had put forth a proposal to cap physician payment. He added: “In addition, we are not looking to change the end-of-life care benefit that we feel is so valuable to our community. Unfortunately, wherever this information came from is inaccurate and hopefully unintentionally misinterpreted.” Dr Brathwaite said that the BHeC had a “very productive relationship with all health providers, including physicians”. He added: “The BHeC is continuing to ask physicians how we can best include more primary care and prevention for all into our accessible health system.” A spokeswoman for the Ministry of Health said yesterday that it had been in “active dialogue” with stakeholders about reform to Bermuda’s health financing system. “End-of-life care has not been addressed specifically, but we are pleased that hospice and home palliative care is already covered as a Standard Health Benefit under the current minimum insurance package. This benefit is not under discussion.” The spokeswoman said the ministry would be in a position to share more details on health financing reform “in the coming months”.
2019. June 13. The Ministry of Health announced a plan of action today to encourage Bermudians to receive vaccination shots. Kim Wilson, the health minister, said that Bermuda’s Strategy on Vaccination Hesitancy would aim to increase Bermuda’s vaccination coverage by 10 per cent by 2021. The plan was put together after the ministry conducted research on the delay or refusal of vaccinations. Ms Wilson said health officials would:
Ms Wilson announced her intention to increase vaccines for children under the age of six months in April. She said that the number of children who received the measles, mumps and rubella vaccine had dropped to 87 per cent — below the 95 per cent global target. Ms Wilson added yesterday that the decreased global target, when combined with our status as a popular travel destination, made Bermuda more vulnerable to outbreaks of disease. She said: “Not only is measles at our doorstep, being one flight away considering the recent outbreaks in New York City, but also because in Bermuda we have detected high levels of vaccine hesitancy, which means that not enough people have been vaccinated to give our people herd immunity.”
Ms Wilson issued the following advice:
2019. June 10. A number of factors including Brexit could be driving up prices on some prescription drugs in Bermuda, it is feared. Pharmacists said medication recalls and manufacturing issues also played a part, after one patient reported that the cost of his treatment had soared by more than five times. A wholesaler explained that it was not unusual for access to supplies to be limited by events in other countries. The Bermuda Health Council confirmed it was aware of challenges and hoped to improve the prescription drug industry “in the near future”. One drugstore customer said: “I went to renew a prescription and the cost of the prescription that I normally obtain had risen from $13 to $71. The pharmacist actually drew my attention to it, explaining that this was an impact of the Brexit events, that their supplier in the UK was stocking up on this particular type of medication and was not able to provide it, so they had to source it from the US initially and that resulted in the increase in cost. Given that people were interested in the cost of health at the moment, I thought this is something that was a bit beyond the reach of our government to control.” The Government Employee Health Insurance scheme member wrote to Kim Wilson, the Minister of Health. A health ministry spokeswoman confirmed that the customer’s concern had been raised. She added: “We are observing the situation as it has not been a problem across the board.” Ricky Brathwaite, the BHeC acting chief executive and health economics director, said: “The health council is aware that there are sometimes challenges with getting prescription medications from the international market. As a small country with a population of 63,799, Bermuda is sometimes not the priority for the manufacturers and suppliers that have the inventories. And to make the situation even more complicated, when there are times when the world is buying up certain medications because of political or economic uncertainty, the demand leads to higher global prices. During those times we do not have the buying power by ourselves to combat those increases in prices or the ability to negotiate to the best of our ability because of the relatively small quantity of those medications we want to purchase.” Dr Brathwaite said the council’s recommendations included consolidating orders and reducing an “affinity” towards brand name medications. He added: “We understand that many of the issues in the world are out of our direct control. The council will continue to work with our pharmacist, hospital and physician partners to make improvements to our prescription medication industry in the near future so that we can do our local part to reduce the costs of medications to our consumers and their families. We will also work with our international partners ... on better procurement strategies to mitigate the roller coaster that can exist in medication pricing.” David Ugwuozor, the Bermuda Pharmaceutical Association president, believes stockpiling took place before the original date for the UK’s exit from the European Union, which was March 29. He added: “In Bermuda, people did buy in anticipation that Brexit was going to go wrong.” The pharmacist at Robertson’s, in St George’s, said: “I don’t think it was everyone, but some pharmacies did panic buy for sure — the last thing we want is to be short here.” Mr Ugwuozor explained that the UK sourced much of its medication from Europe, so changes in regulations, tariffs or trade relations could affect the purchase of drugs, which would create problems for Bermuda because it orders from the British market, among others. He added: “We’re a small island, the knock-on effect would be significant.” Mr Ugwuozor said various factors appeared to be affecting a number of drugs. “This fluctuation is quite bad for the patients, especially if they’re struggling to pay, so I can understand the concern. They would not really understand why it’s happening ... not just Brexit, there are tons and tons of issues — supply issues, manufacturing issues, stockpiling — those are just three factors that would affect distribution of drugs, which in turn affects price.” He added that concerns had been raised with the BHeC and the industry would keep watch in the coming months as the new Brexit date of October 31 approaches. A UK Department of Health and Social Care spokeswoman said that “robust contingency plans” were in place and if they were followed there should be no interruption to medical supplies when the country leaves the EU. She advised that suppliers were asked last August to stockpile six weeks’ supply on top of their usual buffer stocks ahead of a possible “no deal” Brexit but that should not impact the ability to meet demand from other countries. Jon Turner, who covers pharmaceutical supplies at BGA Wholesale Distributor, said: “There’s always something that’s causing problems for supply for pharmaceuticals to Bermuda. We have had challenges and we have done our best to divert supply to other jurisdictions to resolve those.” It was unclear if disruption caused by Brexit was the cause. Mr Turner explained: “I wasn’t really getting a specific message from my suppliers, the order comes through unfulfilled so BGA, with it’s experience and expertise, makes alternative arrangements as best as we can to maintain supply for pharmaceuticals in the community, but that can be a demanding task. I would say it’s the normal ebb and flow of supply.” Terry-Ann Waite, at People’s Pharmacy, said the issues were also linked to “global shortage and several manufacturing companies having problems with their plants”. She added that the FDA had recalled some hyper- tensive medication, which had become “extremely hard” to source. Ms Waite said: “For the ones you can get, the prices have gone up.” Although a finance ministry spokeswoman said the GEHI scheme had no “specific carve-out” for generic prescription medication, the programme’s benefits schedule suggested policyholders paid 20 per cent of the total cost. In comparison, most Argus, Colonial and BF&M policyholders are covered 100 per cent for generic prescription drugs and 80 per cent for brand name medication. An Argus spokeswoman said: “While we generally see an upward trend in medication costs, we have yet to experience any unusual spikes in our prescription claims.” A BF&M spokeswoman added that the company was not aware of cost increases that could be attributed to Brexit.
2019. June 6. The Bermuda Health Council issued this press release. "Today, the Health Council launched a campaign #ImagineBermuda, about their vision of Bermuda’s health system. The campaign provides a timely reminder that the youngest and the oldest amongst us can still impact and even create the Bermuda we want to see for tomorrow. We want to give Mr and Mrs Bermuda, and all Bermudians alike, a voice to shed light on the many issues and opportunities within our communities. This is a great opportunity for everyone to promote their hopes and dreams; and a great opportunity for our kids, youth, adults and seniors to share their version of an economically strong and healthy population. The campaign encourages members of the public to create and post a social media video, no more than 60 seconds, about what they imagine for the future of Bermuda. This video does not have to focus solely on the health system but rather any hopes you have for making this the best Bermuda, for all. To learn more about the Health Council’s campaign, visit their Facebook @BDAHeatlhCouncil or Instagram page @BDAHealth."
2019. June 3. An interactive wellness programme for government employees will be launched next month in an effort to tackle the $12.8 million cost of public sector sick leave. Workers were urged to take on the team-based challenge as part of a Throne Speech pledge that would place them at the front of a “strategic plan to halt the rise of obesity and diabetes in Bermuda”. A Cabinet Office spokeswoman explained that 42,681 days were lost through illness last year, after employees each took an average of 9.6 sick days, and the figures were unsustainable. Covering food choices, exercise, sleep and stress management, the scheme will be the first of its kind in the island’s public service and is designed to develop long-lasting habits in a “culture of wellness”. The spokeswoman said: “We must find ways to encourage healthy lifestyle choices and do all that is necessary to help make the more than 4,000 public officers as healthy as possible.” She explained that in 2017 the Progressive Labour Party administration’s Throne Speech vowed: “The Government will engage all sectors of society in a coordinated, strategic plan to halt the rise in obesity and diabetes in Bermuda. The Government will lead the way in wellness by encouraging its employees to make healthy choices, and will contribute to their wellbeing by offering programmes, incentives and education to support the journey to a healthier public service.” An employee wellness committee was set up last year and members carried out “extensive research” before they settled on a scheme that addressed the needs of their island-wide colleagues. The spokeswoman said that the cost of certified sick leave in 2018 was $9,687,287, with the Government’s 4,455 employees each taking an average of 7.2 paid days. Uncertified absence through illness was found to be worth $3,115,304, accumulated by an average of 2.4 days per worker. Government Employee Health Insurance claims amounted to $63 million, the spokeswoman added. She said: “The health-related numbers within the public service are unsustainable and must be addressed from the front end.” The spokeswoman added: “If you look closely at the numbers you will see that more than $9,600,000 was spent on certified sick days. This is indicative of an ageing workforce together with employees who have long-term illnesses. Our goal is to reduce these numbers by improving employees’ health.” She said the wellness committee, with the support of Derrick Binns, the head of the public service, and senior managers — introduced a Wellness in 2019 programme with a yearlong Global Challenge that will start with a “kickoff event” for participating staff members on July 10. Teams will be made up of seven people, and the cost of $113 per head can be shared between the participant and the Government. The spokeswoman added: “For 31 cents a day, we hope to see small changes in participants’ health. Through the programme they will learn to make healthy food choices, understand the importance of adequate sleep, increase physical activity and begin to effectively manage stress, among other sustainable lifestyle choices. This is an important step for the public service. We want to create a culture of wellness. While there have been other options in the past, this is the first time we are introducing a holistic approach to managing the health of employees.” The Global Challenge programme is run by Virgin Pulse, which is part of Sir Richard Branson’s Virgin Group and “designs technology that cultivates good lifestyle habits for your employees”, according to its website. It explained: “For over 15 years, this 12-month programme has been improving lives, boosting culture and camaraderie, increasing job satisfaction and productivity and reducing employee stress levels. Through an immersive and engaging experience, the Global Challenge addresses key elements of employee wellbeing including physical activity, nutrition, sleep and mental wellbeing.” The website said that the team aspect created “healthy competition”, a support network and provided accountability. Group members will each receive a starter kit that includes a Max Buzz activity tracker to monitor steps, sleep and the number of calories burnt. Employees will find out how to assess their own health as they embark on the programme and will be able to measure their progress. The Virgin Pulse website added: “Real-time reports allow employers to monitor overall health improvements across their workforces.” Public servants will have access to an online platform and a smartphones app where they can take advantage of tips and advice and share their experiences with others involved in the scheme all over the world. The Bermuda Government spokeswoman said employees still had time to sign up and should contact their head of department to show their interest. She added: “With the introduction of this healthier living lifestyle tool, we anticipate public officers will, over time, adopt healthy choices.” The sick leave total value of more than $12.8 million was an increase from the sum revealed in the 2013 Sage Commission report on spending and government efficiency, which said that employees’ illness rates cost more than $10 million a year. It said then that Bermuda public workers took an average of eight days off sick annually.
2019. June 1. Opinion. By Craig Cannonier, MP, Leader of the Opposition and the MP for Devonshire South Central (Constituency 12). "Today the Government will effectively go into the healthcare business. It has been a rushed process and its consequences were not thought through. Why rushed? There were only a few weeks separating the introduction in the House of Assembly of the Health Insurance Amendment Act, which changes the way healthcare has been funded for decades, and its date to come into effect. The insurance companies all complained about a lack of proper consultation and there were a couple of public meetings, one of which was held at an apolitically neutral location. The result has been confusion among Bermudians about what is happening, why, and its impact on them and their wallets. In addition, the subject of a $65 million fund as back-up should the Bermuda Hospitals Board spend its full $330 million grant was introduced only the night before this legislation was debated in the House. It meant there were many unanswered questions — for instance, how is this $65 million going to be funded? Given that the latest BHB report from 2013-14 has only just been tabled in the House, how do we know if the right checks and balances are being applied? Will we be told how pricing is being calculated? How will we know if all of the $330 million is being apportioned to healthcare in a cost-efficient way? For an issue as important and as complex as healthcare, the rush in passing this legislation looks like an attempt to railroad something through — never mind the consequences. Bermudians have every right to be angry about these tactics. Just because the Government has a large majority, it does not mean it should be allowed to ride roughshod over the people. That is supremely arrogant. One of the consequences of rushing legislation is that its implications are not fully considered. Whatever the Government says, whatever the reasons given, people are not seeing healthcare premiums decreasing. This affects those in the private sector much more than in the Civil Service and is in contradiction to the Progressive Labour Party’s promise to lower the cost of living, notwithstanding the pledge to reduce healthcare costs. As a result, yet another burden is being added to the increasing woes of businesses and Bermudians. On top of things such as the sugar tax, the dividend tax and the increased land tax, banks are passing on the cost of the increased charges that were levied by the Government in the last Budget and charges are now being passed to Bermudians paying their tax with a credit card. At the same time, there is no sign of the Government reining in its spending and, while fintech may eventually produce jobs, it is not going to do so anytime soon, nor with the kind of numbers we need. There appears to be no Plan B. That leads to the other key issue here: the need for more people on the island to increase the pool and spread the cost of healthcare. Despite the Immigration Reform Group’s report being tabled almost 18 months ago, the Government is yet again asking for feedback and engaging in even more consultation. It is clearly all at sea over this and cannot reach a solution that satisfies different factions within Cabinet and the party. We are on course to spend $1 billion a year on healthcare, the burden of which will fall on fewer, and older, people unless the population is increased. The $1 billion figure is staggering for a population of some 60,000. Why are we heading there? It’s largely because of overuse of medical services — a crucial issue that this government has done nothing to address. We are approaching a tipping point, with our future uncertain as the burdens being placed on Bermudians increase. I am very concerned for my country."
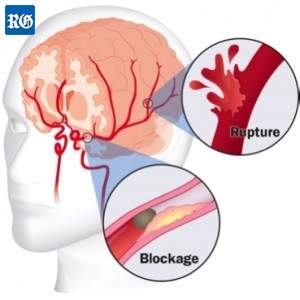 2019.
May 29. A specialist stroke centre is to be opened at the King Edward VII
Memorial Hospital. A spokeswoman for the Bermuda Hospitals Board said four
to five Bermuda residents suffered a stroke every week — between 208 and 260
people a year. The KEMH unit is to be opened in partnership with Maryland-based
Johns Hopkins Medical. Victor Urrutia, of Johns Hopkins Medical, said a stroke
unit in Bermuda could reduce mortality and disability. Dr Urrutia added that
stroke units had been proved to cut deaths by at least 14 per cent and the
number of people left disabled by a stroke by 18 per cent. He said KEMH already
had the staff and equipment to do the job, but the Johns Hopkins team would
provide expert guidance on how to best treat stroke victims. Dr Urrutia
explained that all healthcare staff involved in the recovery of stroke patients
would work together to ensure the best treatment possible. He said: “We will
develop a protocol to ensure that all patients are treated faster.” Dr Urrutia
added that treatment of a stroke patient worked better the faster it was
administered. He said: “Bermuda is already taking care of stroke patients, but
we will enhance the process so we can formally work as a stroke centre. The
hospital is ready to become a stroke centre.” Dr Urrutia added: “We will be
measuring the outcome and process on an ongoing basis so it can be optimized and
improved.” He said the collection of information would allow healthcare staff
to assess how effective the process was and help improve the level of care for
patients. He added that the risk factor for a stroke was high in Bermuda because
about 20 per cent of the population was aged over 65. Dr Urrutia said: “The
older you are, the more likely you are to have a stroke.” Strokes can affect
anyone, but those who have high blood pressure, heart disease, are obese, smoke
or use illegal drugs run a higher risk. Studies have found that black African,
black Caribbean and people of South Asian origin on average suffer strokes ten
years earlier than white people. Strokes are the second biggest cause of death
worldwide.
2019.
May 29. A specialist stroke centre is to be opened at the King Edward VII
Memorial Hospital. A spokeswoman for the Bermuda Hospitals Board said four
to five Bermuda residents suffered a stroke every week — between 208 and 260
people a year. The KEMH unit is to be opened in partnership with Maryland-based
Johns Hopkins Medical. Victor Urrutia, of Johns Hopkins Medical, said a stroke
unit in Bermuda could reduce mortality and disability. Dr Urrutia added that
stroke units had been proved to cut deaths by at least 14 per cent and the
number of people left disabled by a stroke by 18 per cent. He said KEMH already
had the staff and equipment to do the job, but the Johns Hopkins team would
provide expert guidance on how to best treat stroke victims. Dr Urrutia
explained that all healthcare staff involved in the recovery of stroke patients
would work together to ensure the best treatment possible. He said: “We will
develop a protocol to ensure that all patients are treated faster.” Dr Urrutia
added that treatment of a stroke patient worked better the faster it was
administered. He said: “Bermuda is already taking care of stroke patients, but
we will enhance the process so we can formally work as a stroke centre. The
hospital is ready to become a stroke centre.” Dr Urrutia added: “We will be
measuring the outcome and process on an ongoing basis so it can be optimized and
improved.” He said the collection of information would allow healthcare staff
to assess how effective the process was and help improve the level of care for
patients. He added that the risk factor for a stroke was high in Bermuda because
about 20 per cent of the population was aged over 65. Dr Urrutia said: “The
older you are, the more likely you are to have a stroke.” Strokes can affect
anyone, but those who have high blood pressure, heart disease, are obese, smoke
or use illegal drugs run a higher risk. Studies have found that black African,
black Caribbean and people of South Asian origin on average suffer strokes ten
years earlier than white people. Strokes are the second biggest cause of death
worldwide.
2019. May 23. Controversial changes to healthcare financing were passed in the Senate yesterday after two government senators who had excused themselves because of illness returned for the vote. The Health Insurance Amendment Act was resisted by the three One Bermuda Alliance senators, including Nick Kempe, the Senate Leader, who said it was “rushed” and ineffective. The legislation was passed after Jason Hayward and Kathy Lynn Simmons attended the debate, despite illness. Joan Dillas-Wright, the Senate president, said they “got out of their sickbeds to come and support this Bill”. Mr Kempe’s motion to delay the second reading of the Bill was also voted down five to four. He argued that there had been insufficient time to consider the Bill, which was passed by the House of Assembly last Friday. Mr Kempe’s motion was supported by James Jardine, an independent senator, as well as the Opposition, but defeated by the government side. The Bill was drawn up to allow the Government to pay an annual grant to the Bermuda Hospitals Board, capped at $330 million for the coming year, to replace the existing fee-for-service arrangement under the Health Insurance Amendment Act. The block payment will be funded by the Government with a more than threefold increase in the amount it takes from monthly premium payments to health insurers, up from $101.97 to $331.97. The legislation will come into effect on June 1. Anthony Richardson, a Progressive Labour Party senator, earlier tabled the Bill on Mr Hayward’s behalf. Mr Richardson said the changes to hospital financing would head off an estimated $20 million increase in healthcare costs. Marcus Jones, an Opposition senator, said the Bill had been brought to the legislature with “speed and reckless abandon”. Mr Jones added the legislation failed to tackle rising costs. He said: “That is where the health costs really hit the Bermudian public really hard.” Mr Jones added there had been a lack of consultation with insurance companies. Mr Jardine warned that there would be no savings if the hospital over ran its $330 million budget. He also read out a letter he had received from the Association of Bermuda International Companies, endorsed by the Bermuda Chamber of Commerce, the Bermuda Employers’ Council, and the Bermuda Hotel Association, that asked him to push for a rethink on the changes. Michelle Simmons, an independent senator, said the Government should “go further” instead of “tinkering with one part of the system”. Mr Kempe said the legislation would not cut costs or bring the island closer to universal health coverage. He added: “This simply transfers negative claims from the Government’s books to the private sector’s books”. Mr Hayward said the legislation was the first in a series of moves to “change our broken system”. Opposition senators tried to delay approval of the Bill until the next sitting of the Senate on June 5. Independent senators sided with the Government on a final vote, and the Bill was passed by seven votes to three.
2019. May 22. An expert on diabetes has been appointed as a consultant endocrinologist by the Bermuda Hospitals Board. Andrew Jamieson, from, Glasgow, Scotland, previously worked to tackle the disease in the United Arab Emirates. Dr Jamieson said: “I am looking forward to serving the community and working to improve health outcomes for diabetics in this beautiful island.” He will replace Annabel Fountain, who was director of endocrinology until the end of 2017. Diabetics in Bermuda have an average age of 57, eight years younger than in Britain. Health experts have warned the diabetes rate is increasing because 74 per cent of the adult population is overweight or obese. Dr Jamieson, who came top of his class at the prestigious Glasgow University medical school, has been appointed on an initial two-year contract. He trained in endocrinology in Glasgow and worked as a consultant endocrinologist for NHS Scotland for 17 years before he became deputy medical director of the Valiant Clinic in Dubai. He has also authored many published articles on clinical aspects of diabetes, endocrinology and osteoporosis. Michael Richmond, the BHB chief of staff, said: “We are fortunate to have Dr Jamieson join the BHB team. His knowledge and expertise in diabetes and his experience in managing the disease in Dubai, a high-diabetes-prevalence area, will benefit the entire Bermuda community.”
2019. May 20. A controversial Bill to change how Bermuda’s hospital is funded was passed last night. The Government is to pay an annual grant to the Bermuda Hospitals Board, capped at $330 million for the coming year, to replace the existing fee-for-service arrangement under the Health Insurance Amendment Act. The block payment will be funded by the Government with a more than threefold increase in the amount it takes from monthly premium payments to health insurers, up from $101.97 to $331.97. Kim Wilson, the Minister of Health, said that the hospital would be held “more accountable” in return for the cash. She added that the Government wanted “better efficiencies and better health outcomes”. Ms Wilson said: “We are demanding the best from our hospital and they are taking the progressive and responsible steps to achieve under those demands.” She said that the Government was also asking insurance companies to “conduct business differently”. Ms Wilson added: “We are looking for each of those companies to use more of the money you are paying in health insurance premiums to pay for your health. We are demanding to put the health of people as a higher priority to the health of profits.” Patricia Gordon-Pamplin, the shadow health minister, said the Bill would “turn the healthcare system on its head as we know it”. She added: “I believe it deserves more than the short shrift that the Government has afforded it in trying to railroad this legislation through within one week.” Ms Gordon-Pamplin said that insurance industry representatives that she had spoken with described consultation with the Government on the changes as “woefully inadequate”. She added that the country’s need for quality healthcare would not be achieved through the legislation. Ms Gordon-Pamplin added: “We will see that there will be more expense, in terms of premiums outside of the standard health benefit, there will be no guarantees for efficiencies, and there will be no guarantees for positive health outcomes.” Wayne Furbert, the Minister for the Cabinet Office, called the arguments made by Ms Gordon-Pamplin “weak”. Mr Furbert said that the legislation was “the first step” as part of the Government’s promise to lower healthcare costs. He added: “Is this the final stage? Nope, it’s part of the beginning of where we are headed.” Craig Cannonier, the Opposition leader, questioned how the Bill would combat high costs. He added: “We haven’t heard that. We still have not answered the question of how are we lowering insurance costs for Bermudians.” Tinée Furbert, a PLP backbencher, said healthcare had been allowed to become a “business of profit. We have to try to figure out how to pull in the reins now, if we don’t we are going to be in big trouble Bermuda.” Ms Furbert urged the island’s residents to “shop around” for healthcare needs. Michael Dunkley, an Opposition backbencher, called the Bill “Sugar Tax No 2”. He added: “Sugar Tax No 1 was well-intentioned. Sugar Tax No 1 was done without adequate consultation, no listening, just advising.” Mr Dunkley said that the Government was “quietly and conveniently putting an increased burden on the private sector”. He added: “This Bill does nothing to address the fundamental cost of healthcare in Bermuda.” David Burt, the Premier, said the Bill was a “monumental step. Transformational change is what this government was elected to bring, and that is what we will bring to Bermuda.” Mr Burt said that improvements would not happen overnight. He added: “This is the first step to providing a healthcare system that puts the people’s interests over the interests of people’s profits.” The Bill was tabled last Friday. The new system is scheduled to take effect on June 1.
2019. May 17. A $65 million reserve fund will be available for the hospital if costs run over the block grant to be provided by the Government, a public meeting heard last night. Jennifer Attride-Stirling, the Permanent Secretary of the Ministry of Health, said she hoped the cash would not be needed and was confident the provider would work within its budget. She was on a panel with Kim Wilson, the health minister, and Ricky Brathwaite, the acting chief executive of the Bermuda Health Council, at a meeting about changes to healthcare financing expected to be introduced on June 1. The Government is to pay an annual grant to the Bermuda Hospitals Board, capped at $330 million for the coming year, to replace the existing fee-for-service arrangement. Ms Wilson explained that the money is to be drawn from the Mutual Reinsurance Fund. The Government will boost the MRF because it will more than triple the amount it takes directly from monthly premiums paid to health insurers from $101.97 to $331.97. Ms Wilson added: “The administration and profit is nil, so, effectively, what we’re doing from June 1 is that the Standard Health Benefit premium will be spent on your healthcare.” James Jardine, an independent senator who was among about 70 people at the meeting at St Paul AME Centennial Hall, asked where additional funds would be found if hospital costs exceeded the $330 million grant. Dr Attride-Stirling replied that it would take about a year to determine an amount that allowed “some flexibility up or down, so that the hospital is not bearing such risk”. She added: “But for this fiscal year we, together with the hospital, are confident of the figure and in the event of any slight slippage or discrepancy, the hospital has $65 million in surplus that may be required to be used. We certainly hope that’s not the case.” She said that in the event of a national catastrophe or pandemic “of course the Government is going to step in”. A member of the public earlier asked if patients would be affected due to the fixed budget. Dr Attride-Stirling said: “No ... the $330 million revenue target was agreed very carefully with the hospital to make sure that, over the next fiscal year, they could continue to provide the services they have been and we are absolutely confident of that.” Dr Brathwaite explained that a block grant method could curb overutilisation of services. He said: “It is a fundamental part of fee-for-service systems that you are going to utilize additional things because it is advantageous for you to get more revenue for doing more things. It is not a secret that within fee-for-service systems, whether it be here in Bermuda or other places in the world, that there are unnecessary things that are done, there are admissions that are made to the inpatient wards that are unnecessary because they pay higher amounts of money, but that is the business of healthcare.” He said the island’s system had been based on this way of working for “a very long time”. Dr Brathwaite added: “It doesn’t help from a clinical standpoint, it helps from a business model so we are now putting constraints on the system and saying, look, this has to be about healthcare; this has to stop being about business.” He said: “This cap incentivise people to do the right thing and to be more efficient in the care that they’re giving.” The panel was asked about the extent to which insurers will obtain information about the services used by their policyholders. Dr Brathwaite told the meeting there had been “some misinterpretation” of talks with the industry over the past two months. He said: “From the very beginning, our objective was always to make sure that each insurer had all the data that they currently are accessing from the hospital. There was some confusion within the ranks of insurers as to whether they wanted the data or not, considering the change in the mechanics. We have settled on, weeks ago, that everyone is going to have access to their data based on the services that their clients get in the hospital.”
2019. May 15. A call by a patients pressure group for the head of the island’s health watchdog to be replaced by a “neutral” non-medical figure has been rejected by the health minister. Kim Wilson said it was “entirely appropriate” for a physician to chair the Bermuda Health Council after the Bermuda Healthcare Advocacy Group questioned whether ophthalmologist Alicia Stovell-Washington should be in the top role. The call came after a member of the public complained to the patients group about being charged for a visit to Dr Stovell-Washington’s surgery when the doctor was not present and other staff conducted tests. The patient, who asked not to be named, said they were surprised to be charged a “substantial” copay for the visit and told they would have to return to see the doctor to have their eyes dilated at further cost. The BHAG said it was difficult to see how the patient could have any confidence in the Bermuda Health Council to investigate the concern, as Dr Stovell-Washington was its chairwoman. But Ms Wilson, who appoints the council’s board, said there was “nothing unusual” about a physician heading up the council. She added: “This is not the first time the health council has had a physician as its chairman and it is entirely appropriate, just as the chair of the Medical Council is a medical doctor and the chairs of other professional councils are health professionals. Dr John Cann was chairman of BHeC in 2012. There is also precedent of a healthcare provider as a chair of the health council, as was the case with Simone Barton of the Bermuda Heart Foundation in 2015 to 2017.” Ms Wilson said she was aware that the health council had rules to deal with potential conflicts, including a conflict-of-interest policy and signed declarations. She added: “I fully support the chairman’s integrity and transparency. The allegations regarding billing have not been raised with me at any time by the Bermuda Healthcare Advocacy Group or by anyone else. As a general rule, complaints about healthcare billing should be raised with the provider directly in the first instance and, if unresolved, can be submitted to the health council by the patient. To my knowledge, no such complaint has been made. If it is, my expectation is that it would be investigated as with any other complaint.” Ricky Brathwaite, the acting chief executive of the BHeC, said the council’s board did not deal with specific complaints so no conflict would arise if a complaint was filed. He added: “No one is provided preferential treatment in the health system. The healthcare advocacy group is more than welcome to file a complaint. Every provider, even Dr Stovell-Washington, would have to go through responding to that complaint if it’s made.” He said physicians were regulated by the medical council and the health council had oversight of insurance matters. Dr Stovell-Washington said in an e-mail: “I have contacted Bermuda Healthcare Advocacy Group and discussed their concerns. The matter has been resolved between us. I ask that the one patient who had a concern contact my practice directly so we can review their inquiries.” The patients group said in a statement that the issue they raised had been “heard, addressed and hopefully resolved”. It added: “Bermuda Health Advocacy Group ... agrees that there should be physicians on the Bermuda Health Council to give valid input. However, senior positions should remain neutral.”
2019. May 13. Annual reports for the Bermuda Hospitals Board, which have lagged at the Auditor-General’s office, will “soon be completely up to date”, the health minister pledged. Kim Wilson tabled the BHB’s annual report for 2013-14 in the House of Assembly on Friday. Ms Wilson told MPs that the five outstanding reports would be published over the course of “the coming financial year”. In her preamble to the 52-page report, Ms Wilson said that “a lot of accomplishments” were marked by BHB that year, “including improvements in patients’ experience, preparing for the opening of the new Acute Care Wing, and careful management of public monies — securing a $46.6 million surplus to reinvest into the hospitals’ infrastructure and Bermuda’s health system”. She added: “The Government is proud of our country’s hospitals and indebted to the 1,800 dedicated staff at King Edward VII Memorial Hospital and Mid-Atlantic Wellness Institute who serve our community selflessly — particularly in times of emergencies. We are indebted to the executive team leading BHB’s ongoing improvements and cost-containment initiatives.” Ms Wilson also thanked the board that served at the time for “overseeing enhancements in governance and policy for the hospital’s leadership”.
2019. May 10. The former chief executive of the Bermuda Health Council claims in an application for judicial review pending before the Supreme Court that the Premier interfered in the running of the watchdog to push taxpayer-funded payments to Ewart Brown. Tawanna Wedderburn alleges in the proceedings that intervention by David Burt also benefited at least one Cabinet minister and some Progressive Labour Party supporters. She also claims as part of the proceedings that Kim Wilson, the Minister of Health, and Alicia Stovell-Washington, the BHeC chairwoman, interfered with the day-to-day operation of the council. The notice of application that started the proceedings was released by the court after a formal request from The Royal Gazette. The document was submitted to the court as part of Ms Wedderburn’s attempt to win an order to quash her termination as BHeC chief executive last December. Mr Burt said last night: “The allegations are strongly denied and they will be defended in the appropriate forum.” A Ministry of Health spokeswoman added that the respondents in the case “vigorously denied” the allegations and were “robustly” defending themselves in the proceedings. The case started with a hearing last week in chambers. Ms Wedderburn asked for permission to apply for a judicial review against the three individuals and the council in March, which was granted last month. The application shows that Ms Wedderburn sought relief from what she alleged were “continuing” decisions by the Premier, the health minister and the BHeC chairwoman “to interfere with the functioning and day-to-day management of the Bermuda Health Council”. The application adds that she wanted an order to quash the BHeC’s decision to recommend that she should be removed as chief executive, Ms Wilson’s approval of the recommendation, the termination itself, or all three. Ms Wedderburn also wants a ruling that alleged interference by the Premier and the health minister was “unlawful because the council is intended to be an independent health regulator, performing its functions without party political interference”. But Mr Burt said: “For the avoidance of doubt and for the information of the public, the Bermuda Health Council is not an independent regulator. This statutory body is, by law, subject to the directions of the Minister of Health.” Ms Wedderburn “further or alternatively” asked for the court to rule that the alleged interference by the Premier, the health minister and Dr Stovell-Washington was unlawful “because it was done for the purpose of controlling the council’s policy decisions, and/or facilitating government payments and/or other pecuniary awards to specific Progressive Labour Party supporters, a former premier, at least one Cabinet minister, and/or others”. Ms Wedderburn’s tenure at the BHeC ended in December last year in what the health watchdog said was a “separation of employment”. She served as chief executive for nearly three years and had worked at the organisation since 2007 in other roles. The BHeC is responsible for setting MRI and CT scan charges for private healthcare providers. The former One Bermuda Alliance administration slashed fee rates in June 2017. The cuts affected the King Edward VII Memorial Hospital as well as two clinics owned by Dr Brown, a former PLP premier. Compensation expected to total $3.6 million — $2.4 million to Bermuda Hospitals Board and $1.2 million to Dr Brown — is to be paid out by the PLP government. Records released under public access to information in 2018 by the Ministry of Health showed how Dr Brown, the owner of Bermuda Healthcare Services in Paget and the Brown-Darrell Clinic in Smith’s, sent a string of angry e-mails and letters about the fee cuts to Ms Wedderburn. He also named her and two other public servants when he announced the closure of the scanner unit at the Brown-Darrell clinic because of the fee cuts in January 2018. Dr Brown said at a press conference: “Remember these names. Jennifer Attride-Stirling, Permanent Secretary at the Ministry of Health. Tawanna Wedderburn, CEO of the health council, and Ricky Brathwaite, so-called health economist. I want you to remember those names.” He was not named in the application for leave form that was submitted by Ms Wedderburn, and provided to the Gazette after it asked the Supreme Court registry for access to records, but it is understood he is the “former premier” in the documents. Ms Wedderburn also asked for declarations from the court that the recommendation to terminate her as chief executive was unlawful because the council was “tainted by bias” and that she was not notified of the proposed decision or given the opportunity to make representations on it. The notice added that she wanted: “Further or alternatively, a declaration that the recommendation was unlawful because it was made for improper purposes, namely: because Wedderburn was perceived to be obstructive to certain political intentions; to safeguard a series of unlawful decisions in favour of specific individuals and/or healthcare providers; to make it likely that specific politically motivated policies would be imposed upon the council without any or any adequate obstruction; and/or because of personal animosity against Wedderburn.” It was also alleged that Ms Wilson’s approval was unlawful for the same reasons or because she did not fully investigate the recommendation before it was carried out. Ms Wedderburn claimed that the alleged refusal of permission for her to join a trade union was unlawful and she said she wanted damages “for the Premier’s, minister’s, chairman’s and/or council’s misfeasance in public office”. A Ministry of Health spokeswoman said: “The respondents in this matter vigorously deny the applicant’s allegations in their entirety, and are robustly defending their position through the proper court process, adhering to its rules. Therefore, further comment cannot be made at this time.” Juliana Snelling ,of Canterbury Law, who is acting for the BHeC and Dr Stovell-Washington, said it was “entirely inappropriate” for the council or the chairwoman to comment as the case was before the courts. Canterbury Law said in January that Ms Wedderburn’s employment was “terminated lawfully by the council in full compliance with section 18(1)(b) of the Employment Act 2000, the Bermuda Health Council Act 2004 and her contract of employment which calls for one-month notice of termination”. The BHeC lawyers added that Ms Wedderburn was paid for her notice period and also offered six months’ pay and benefits “in good faith”. Eugene Johnston, who represents Ms Wedderburn, declined to comment.
2019. May 9. The Bermuda Government’s singling out of BF&M for criticism over health insurance premium increases is clouding the bigger picture of the ramifications of healthcare financing reform. That is the view of BF&M executives, who said there was much uncertainty about how the new system would work, with just 3½ weeks to go before its planned implementation. Kim Wilson, the health minister, said last week that it was “unconscionable” that BF&M should blame the impact of government reforms for an increase in premiums. She added that a letter from BF&M to clients was “misleading” and inaccurate. In an interview, John Wight, BF&M’s chief executive officer, said the letter to clients was intended to clarify what went into premium rate decisions. “Our primary objective was to educate our customers,” Mr Wight said. “This is a normal part of our discussion with clients and we want to be fully transparent.” He added that the imminent reforms did nothing to address the drivers of healthcare cost increases. A new system for funding the hospital is scheduled to kick in on June 1. It involves the Government paying an annual grant to the Bermuda Hospitals Board, capped at $330 million for the coming year to replace the existing fee-for-service model. Mr Wight said there seemed to be a lack of understanding in the healthcare industry about how things would operate under the revamped system. To fund the block hospital payment, the Government will more than triple the amount it takes directly from the monthly premiums paid to health insurers from $101.97 to $331.97, with the proceeds going into the Mutual Reinsurance Fund. BF&M has characterized this as an “indirect tax”, a description Ms Wilson rejected. Michelle Jackson, BF&M’s senior vice-president, group lines health and life, said public discussion should not focus on the Government’s attack on BF&M. “There is a much, much bigger picture,” Ms Jackson said. “There are wider questions about the $330 million cap and what happens as healthcare costs continue to go up and what that means for future years.” The Government had informed BF&M of the planned financing reforms only about three months ago, she said, and now the reforms were just weeks away from being implemented with much uncertainty about many aspects. Ms Jackson said under the present system, insurers manage and process their clients’ hospital claims. This gives the insurer data, allowing them to analyze trends, as well as creating a check and balance in the system to ensure treatment of their clients is appropriate and efficient. Under the new system, insurers will no longer manage claims or receive information on claims from the hospital when its clients receive treatment, according to Ms Jackson. Ricky Brathwaite, the acting chief executive of the Bermuda Health Council, said last week that insurers would receive data on their clients’ hospital care. Ms Jackson said BF&M had received no guidance on what claims data would be shared. She said health insurance premiums include two components. First, the standard premium rate, which is set by the Government and which covers most hospital services, diagnostic imaging and support of government-administered plans. This component is made up of the standard health benefit, managed by insurers, and the Mutual Reinsurance Fund contribution, paid straight to the Government. Under the reforms 93 per cent of the SPR will go to the MRF, leaving just $23.34 of the total $355.31 be. The second component is comprehensive coverage, the extra non-hospital benefits provided by insurers on most policies, such as prescription drugs, dental care and mental healthcare. In its letter to clients, BF&M states: “We will be increasing comprehensive coverage premium rates by more than in years past as a result of our significantly reduced SHB premiums (approximately 90 per cent less than current). Given current health trends and healthcare cost inflation, we project premiums will not be sufficient to pay expected claims for 2019-20 without this increase.” Healthcare cost inflation was running at 6.5 per cent, well above general inflation, a rate that would likely accelerate as the population aged, leading to greater use of health services and higher claims, Ms Jackson said. The Royal Gazette approached health insurers Argus and Colonial, asking whether they had increased premiums and for views on Ms Wilson’s comments about BF&M. A spokeswoman for Argus said adjustments to premiums “take into account a number of factors, including but not limited to the rising cost of healthcare”. She added: “As per the Aon 2019 Global Medical Trend Rates Report, global medical inflation is currently trending at 7.8 per cent, however, Bermuda traditionally experiences greater increases due to our high incidence of chronic disease and utilization of services. It is important to understand that adjustments vary by corporate client as they are based on the respective claims experience for each client and their particular benefit package. Regardless of changes to legislation, we know that a healthy lifestyle, supported by healthcare professionals, is the key to keeping premiums low and driving down overall costs.” No one at Colonial was available for comment.
2019. May 8. Stroke patients will have access to “the best possible chance at full recovery”, thanks to a link-up between the Bermuda Hospitals Board and Johns Hopkins Medicine. The move, welcomed as a “dream come true” by campaigners, will see a primary stroke centre established in Bermuda, with accreditation for acute stroke care in place by 2021. The clinical affiliation with the Maryland-based medical institute will also include improvements in psychiatric care, a continuing medical education programme for physicians in Bermuda and a residency programme. Michael Richmond, Chief of Staff at the BHB, told a press conference: “Stroke treatment and rehabilitation is a key focus. We have four to five stroke cases come to the hospital per week. We want to ensure we are giving every stroke patient the best possible chance at full recovery, and also identifying people at risk even earlier to try and prevent one altogether. We are also looking at psychiatry for opportunities to improve and find more effective ways to structure and deliver our services.” Dr Richmond said the aim was to provide treatment that matches “the best of the best”. The agreement with Johns Hopkins will cost $1.6 million over two years. Mark Selley, chairman of the Bermuda Family Stroke Association, said of the plans for a stroke centre: “It would be like a dream come true.” Mr Selley said that he had lobbied for 26 years for a stroke unit that also deals with road traffic accidents and neurological problems, but that they were “placed on the back burner”. He added: “I am happy to see this arrangement. If the BHB can team up with Johns Hopkins, we would be so far ahead in the game.” Mr Selley pointed out that the longer it took for stroke patients to get the help needed, the less likely they were to recover. He said rehabilitation by trained specialists was important in the first few days after a stroke. “Like chemo is key to cancer treatment, rehab is key to stroke treatment,” he said. Mr Selley said a local centre that addressed all the needs of a stroke patient would also reduce travel costs. Mr Richmond said quality access to education for doctors was also an important part of the agreement. He said: “Our Continuing Medical Education programme is now accredited by one of the world’s best known and highly respected healthcare providers, and our first CME was held last night.” Venetta Symonds, CEO of the BHB, said: “I’m excited that we are on this journey to improve on-island care for our families, friend and communities with them. It is BHB’s vision to deliver exceptional through strong partnerships and support a healthy community. We ran a robust and lengthy RFP process for our clinical affiliate and six highly acclaimed hospitals applied and went through extensive review. Johns Hopkins won not only due to their quality and status in the healthcare world, but their deep affinity to and understanding of Bermuda.” Mohan Chellappa, executive vice-president and president of Global Ventures, Johns Hopkins Medicine International, said: “We are honored to contribute to the Bermudian healthcare journey. Johns Hopkins Medicine’s mission is to improve the health of the community and the world by setting the standard of excellence in medical education, research and patient care. And the unique community of Bermuda holds a special place in our hearts at Johns Hopkins.” He pointed out that one of Johns Hopkins’ best doctors, Malcolm Brock, was from Bermuda. He said: “We will support BHB staff with education and training and, together, we’re now in the process of establishing a primary stroke centre and preparing for accreditation in the area of acute stroke care in 2021.” The affiliation includes a programme for medical doctors who have graduated from an accredited medical school and are completing additional specialist training at Johns Hopkins. Those doctors will complete four-week rotations to Bermuda to perform short-term clinical and quality improvement projects. Dr Chellappa said: “Our clinical affiliation with Bermuda Hospitals Board is an important part of Johns Hopkins’s vision to enhance healthcare around the world, by sharing our latest clinical advances and research findings in a way that contributes to local healthcare needs and goals, for many years to come.”
2019. May 3. Legal arguments in an action brought by the former chief executive of the Bermuda Health Council against her previous employer were heard behind closed doors yesterday. Tawanna Wedderburn said in March that she had asked for judicial review proceedings against the watchdog, as well as David Burt, the Premier, Kim Wilson, the health minister, and Alicia Stovell-Washington, the chairwoman of the council. A case listed as Ms Wedderburn versus the BHeC and others was scheduled to call in the Supreme Court’s civil jurisdiction at noon. However, after members of the public and media attended, they were advised the case would be heard “in chambers” and open only to the parties involved. The Royal Gazette was unable to obtain information from lawyers after the hearing. Ms Wedderburn’s 11-year career with the BHeC ended last December in what the health council called a “separation of employment”. She said earlier this year that she had received “encouraging messages” from people in the Caribbean, North America and Europe and was “bombarded on the streets of Bermuda with well wishes”. A law firm acting for the BHeC said in January that Ms Wedderburn’s employment was “terminated lawfully by the council in full compliance with section 18(1)(b) of the Employment Act 2000, the Bermuda Health Council Act 2004 and her contract of employment which calls for one-month notice of termination”. The watchdog’s lawyers added that Ms Wedderburn was paid her notice and offered six months pay and benefits “in good faith”.
2019. May 2. Bermuda’s health minister lashed out this morning at a private health insurance provider which she said had raised its premiums. But the president of BF&M said that premium hikes were in part due to proposed healthcare changes by the Government. Kim Wilson said that she had received a letter from a local business sent from BF&M advising that the company was to increase its insurance rates. She added: “It is unconscionable that BF&M, who recently reported heavy profits, would attempt to blame their premium increases on the efficiencies that the Government is making with respect to healthcare payments of our healthcare dollars.” Ms Wilson said that the increase was “significant”. She added: “The letter wrongly blames the Government for the increase. The letter is wholly misleading and contains serious inaccuracies that the public must be made aware of. The standard premium rate and the mutual reinsurance fund premium are not a tax. They are actuarially derived premiums to pay for healthcare. There is no 225 per cent increase on any tax. This is wholly untrue.” She said that the premium increases made by BF&M were a “business decision based on profit margins and shareholder interests. The extra premium they are charging is not to pay for hospital care, because the Government is protecting that by not increasing the standard health premium rate. The extra premiums they are charging is to help to fund profits.” But John Wight, the president and chief executive of BF&M, said that premiums were impacted by several factors “including rising healthcare costs, overall claims experience, as well as the Government’s proposed changes to the distribution of standard premium rate. The proposed Government reform is an exercise in reallocating funds and capping hospital funds, and fails to address the real drivers of the cost of healthcare in Bermuda — the third most expensive per capita in the world. Premiums will continue to increase as a result of our ageing population and the growing number of adults with chronic conditions.” Mr Wight said that the mutual reinsurance fund is embedded in clients’ standard premium rate and that the firm collected it on behalf of the Government. He added: “It is a fact that, as part of the changes to the distribution of the standard premium rate, the MRF is increasing by 225 per cent.” Mr Wight said the firm wanted to work with the Government to develop “thoughtful, comprehensive healthcare reform that achieves our shared goals of stabilizing costs, increasing accessibility, and driving better health outcomes. We are in the process of presenting the Government viable alternatives and we are hopeful that those discussions will result in thoughtful solutions.”
2019. April 29. The number of home healthcare providers has soared, resulting in an increase in abuse of the system, including scams such as time sheets submitted for patients who have died. Kim Wilson, the Minister of Health, revealed the figures last week but said that the incidence of abuse was “low”. She added: “We are looking at further regulations down the line — there is some abuse happening.” Home-care benefits were introduced in 2015 against a backdrop of soaring healthcare costs and rest homes packed to capacity. Seniors in the old continuing care unit at King Edward VII Memorial Hospital were costing the system nearly $14,000 per patient each month. Ms Wilson told The Royal Gazette: “The ethos behind it was to help encourage people to age well at home, and not in the hospital or long-term care facilities. There is a shortage of places and it is expensive for the family.” The minister said that there had been an “exponential” increase in registered carers over the past four years. “It was not anticipated that it would grow quite as fast as it did. It was clear that it was very necessary, but the level of demand generated was much greater than was expected.” Ms Wilson’s remarks came after a town hall meeting on April 15 at Alaska Hall, the Progressive Labour Party headquarters, where she faced questions from carers hoping for an increase in rates. A single mother told her the $15 rate was “crazy”. She added: “I don’t know how I am going to survive.” She also told the meeting that Bermudians were losing out to foreign workers who were “seen as cheap foreign labour”. The minister said last week: “There is a perception that it is employment. But it is not a job — it’s part of the benefit of that particular individual that’s on the Health Insurance Plan or FutureCare.” Ms Wilson said “abuses” had crept in, but that people going on to the programme were being assessed, and that re-registration and greater oversight would cut down on misuse or errors. The ADS register of personal home-care benefit registrants has four categories, with the most basic — personal caregiver — receiving $15 an hour, up to 40 hours a week. Skilled caregivers, able to assist with dementia patients and help with personal care, get $25 an hour to a maximum of 14 hours a week. Registered nurses are eligible for $75 an hour, capped at 12 visits annually. Daycare programme carers, who assist with social activities and recreation, receive $25 per half day or $50 per day, up to $200 a week. Ministry figures up to April 24 show the steep climb in numbers for the first two categories, with the number of new registrants rising virtually every year. There were two personal caregivers registered in 2015, which soared to 299 by this year, with 2018 showing the steepest increase — a jump of 147 new applicants. For skilled caregivers, the nine registered in 2015 has risen to 272 this year. There are 15 registered nurses, as well as 15 home-care agencies, and 20 carers registered for the adult daycare programme. Ms Wilson said it was “an expensive programme to maintain” for those paying the premiums, and emphasised that insurance, not the Government, was footing the bill. But she added: “People are getting cared for that in the past might not have been, and could have ended up in the hospital as a result.” Patients receiving the benefit are assessed first for eligibility, then for the level of care required. She said misuse included examples of time sheets filed that showed suspect hours spent with patients. “You may see a situation where someone has knocked off at 8.30pm in one parish and then started at 8.30pm with another patient all the way down the country. There have also been situations where the recipient of the care has actually passed away.” Ms Wilson said oversight had proved “challenging”, but that “cases are isolated — there is no view that it’s rampant”. She added: “When persons are reassessed, that is when things can get disclosed.” The register of carers is maintained by ADS, and Ms Wilson said there were moves to make it “more readily available for people to search”. She said: “Eligibility criteria are also being reviewed to make sure that the funding available goes to persons most in need. We will be doing that during this fiscal year.”
2019. April 23. Bermuda’s nearly 30-year record of being measles-free could be under threat after a drop in vaccination rates, and a surge in cases abroad, the Minister for Health warned yesterday. Kim Wilson said the number of young children receiving the measles, mumps and rubella vaccine was below the global target — which left the island vulnerable to outbreaks of disease. And she signaled that the Government might consider a mandatory vaccination programme to ensure maximum coverage. Ms Wilson said: “Our excellent track record is no reason to be complacent. Not only is measles at our doorstep, being one flight away considering the recent outbreaks in New York City, but also because in Bermuda we have detected high levels of vaccine hesitancy, which means that not enough people have been vaccinated to give our people herd immunity.” She added that outbreaks of measles in Europe could also be a threat. Ms Wilson said statistics for last year showed increased vaccination rates for some diseases, such as diphtheria, polio and tetanus, in the first six months after birth, which now stands at 95 per cent. But she added there was concern about immunization coverage for the first dose of the MMR vaccine given at 15 months. Ms Wilson explained: “Only 87 per cent of the children at that age received the vaccine, falling below the 95 per cent global target. Low vaccination coverage increases our community’s vulnerability to re-emerging vaccine preventable diseases, such as measles.” There have been more than 17,000 cases of measles in the Americas since 2017, which declared itself measles free in 2016. Measles cases have been reported in countries such as Argentina, the Bahamas, Brazil, Canada, Chile, Colombia, Costa Rica, Mexico, the United States and Venezuela. Ms Wilson said because Bermuda is a major travel destination, there was an increased risk for importation of vaccine preventable diseases. She pointed out that measles was a contagious disease and could quickly spread through Bermuda’s unvaccinated population and cause disruption to schools and businesses. She added that a measles outbreak could also put lives at risk and put extra strain on the healthcare system. The minister said the island had developed a national plan to tackle too low vaccine rates and aimed to increase coverage by 10 per cent by 2021. Ms Wilson added the plan will include the use of a web-based electronic immunization registry to accurately record reporting of immunizations from in the public and private healthcare sectors. She said the plan was backed by the Pan American Health Organisation, which carried out an assessment of the island in February. Ms Wilson added Bermuda would also adopt the World Health Organisation’s guidelines to deal with lower take-up levels for vaccines. She said: “Bermuda and the world are now at risk of diseases which medical science and public health eradicated over a generation ago. “This is a terrible indictment on our population. We must try and we must do better.” Ms Wilson added she got a letter signed by every child medicine specialist in Bermuda last December asking Government to ensure all children had the needed vaccinations by the time they started school. Ms Wilson said that it was “not out of the question” that mandatory vaccinations could be introduced. She added research had shown that fears about health problems as a result of vaccination were unfounded. Ms Wilson said: “I implore all young parents in particular to follow the footsteps of your parents and grandparents, who welcomed preventive measures and made Bermuda free from diseases.” She added the Department of Health will tackle fears over childhood vaccination as part of Vaccination Week in the Americas and World Immunization Week, which both start this week. Ms Wilson said parents and the public could visit health centres this week for updates on vaccine cards.
2019. April 17. A lawyer for patients whose files were seized by police has called for an investigator to be removed from the case over allegations of contempt of court. Mark Pettingill told the Supreme Court yesterday that the police officer approached a patient at her workplace and questioned her. He suggested the officer had accessed medical files — seized in a raid on Bermuda Healthcare Services in Paget and the Brown-Darrell Clinic in Smith’s — despite a court order. But Mark Diel, the lawyer for the Bermuda Police Service, said the officer had approached the patient to find out if patient information had been leaked. Mr Pettingill told the court that last year the officer questioned a patient whose files had been seized as part of an investigation into allegations that the clinics ordered unneeded diagnostic scans. He said the officer had asked the patient if she attended a meeting held about the file seizures and how she had heard about it. Mr Pettingill said the only way the investigator would have known she was a patient was if he had used information in her medical files. He said: “The fact is, he has the knowledge and he’s not supposed to do anything about the knowledge. He cannot utilize it for any purpose. His purpose was to glean further information about the patients whose files were seized. It’s the approach that causes contempt. It’s using the knowledge to go and talk to her.” However, Mr Diel said that the police inspector did not access the woman’s files. He explained that police had drawn up a list of patients who had received a high number of scans before the files were seized. He said: “We are taking all possible steps to protect patient confidentiality. The list that was generated was generated by the police. It was nothing that was seized from the clinics.” Mr Diel told the court the officer had approached the patient about concerns that people whose files were seized had been contacted in breach of an “undertaking” agreement made with the raided clinics. He added that submissions before the court “tacitly admitted” that the clinics had breached the order when they contacted the patients. Mr Diel also argued during the hearing, held in chambers, that Mr Pettingill and Victoria Greening, who also represents the patients in the case, had a conflict of interest. He said Mr Pettingill, a former attorney-general, and Ms Greening, a former Department of Public Prosecutions lawyer, had both received privileged information while in those posts. Mr Diel added that when Mr Pettingill’s and Ms Greening’s Chancery Legal first became involved in the case, it was understood they were focused only on the confidentiality of the medical records. He said that the parties were working to set up a protocol on how the records would be handled at the time. Mr Diel added that if the clinics and Mahesh Reddy, a doctor with the clinics, dropped out of the case because of the protocol, the patients had made it clear they wanted to continue with the judicial review. He said: “Once we knew their intention was to substitute themselves for the applicants, we properly raised the issue of conflict.” Mr Pettingill explained the medical files were not seized until two years after he quit as Attorney-General and Ms Greening had no privileged information on the case. He added that Mr Diel had failed to say what confidential or privileged information either he or Ms Greening had, or how it would benefit their case. Mr Pettingill said: “Patients have a right to privacy of their medical records and our position is the Bermuda Police Service had no right to come and remove them, much less review them. I don’t for a second begin to see where Ms Greening or myself have any type of conflict or advantage in that representation. It cannot be just the inference that we have confidential information or that confidential information was discussed. There has to be the definition of some confidential information and there is nowhere in any of the affidavits that my learned friends indicate what this information is.” Mr Pettingill also argued that it would be “onerous, outrageous and unfair” for his clients to have to find new lawyers after the case had started.
2019. April 15. Health minister Kim Wilson will make a presentation on healthcare costs at a town hall meeting. The Progressive Labour Party’s political education committee is organising the event at Alaska Hall on Monday, from 6pm to 7pm. Ms Wilson has said changes to the island’s health financing would save millions for the hospital while the Government’s mandated premiums remain unchanged. Insurance sources have warned the overhaul effectively shifts costs from government-backed insurance schemes to private healthcare insurance.
2019. April 6. Specialists from the US Lahey clinic who have partnered with the Bermuda Medical Specialities Group pledged yesterday to help tackle the island’s epidemic of diabetes and heart disease. Dinamarie Garcia-Banigan, an endocrinologist, said: “Having the opportunity to practise on the island has enabled me to learn about Bermuda’s healthcare system, Bermudian culture and the services available. A specialist in reproductive health, diabetes, osteoporosis and thyroid disorders, Ms Garcia-Banigan added: “However, wherever you practise, diabetes is a big issue. It’s reflected all over the world.” The BMSG signed an agreement with the Massachusetts-based hospital last month, but Dr Garcia-Banigan said she had been working with the local clinic for two years. She said the arrangement would enable local patients to have access to other Lahey specialists where needed. Dr Garcia-Banigan will visit the island on a regular basis but also use technology to communicate with patients. She added: “I am also planning to build upon my diabetes education programme with one-on-one education.” Michael Levy is a cardiologist and vascular medicine specialist. Dr Levy said his expertise would help fill “a huge need for the island”. BMSG will also offer screening for heart patients — another area of expertise. Both doctors are scheduled to attend a BMSG forum at the Hamilton Princess & Beach Club today. The free event will start at 9.30am, followed by talks at the BMSG clinic on Reid Street, from 2.30pm to 4.30pm
2019. April 5. The public is being encouraged to participate in a survey that could improve care for patients in Bermuda’s health system. The Adverse Childhood Experiences research looks at the link between adverse childhood experiences and the risk of disease later in life. It is hoped that it will lead to better care for chronic conditions such as heart disease, diabetes, obesity, mental health disorders, cancer and asthma. It is being carried out by the Bermuda Health Council in partnership with Family Centre. Tara Hines, the programme manager of data analytics and outcomes research at the health council, said it is hoped 5,000 people will take part. She said, so far, more than 300 people have participated in the research, which started last month and continues until June. Ms Hines added: “We are continuing to increase efforts to have respondents submit their questionnaires, by reaching out to organisations and taking advantage of multiple media outlets, including radio and social media. The nature of this type of information is deeply personal and specific to its respondents and can only benefit from more people being involved. Because this is a countrywide questionnaire, we hope that Bermuda can see this as a community opportunity to be involved and improve our health together.” People of all ages are welcome to participate, particularly adults who lived in Bermuda during any portion of their childhood. Ace research assesses different types of adverse childhood experiences including physical abuse, verbal abuse, sexual abuse, physical neglect, emotional neglect, racism, bullying, poverty as well as family member-related substance abuse, domestic violence, imprisonment, mental illness, negative facets of divorce and death or abandonment. Stephanie Guthman of Family Centre said this research is important for the charity which has been at the forefront of advocating for the issues facing children and families. Dr Guthman said: “The concept of unresolved trauma, also known as Adverse Childhood Experiences, and its consequences has continued to evolve and become increasingly apparent in our communities for more than twenty years. The time is now ripe for Family Centre to continue this momentum and, along with the Bermuda Health Council, we aim to shed light on what Ace and the effects of Ace look like in our community. A major strength of the current study is the opportunity to explore the impact of Ace in a unique and insular population and to do so in a manner that is comprehensive and informative.” Dr Guthman said people have been responding to the survey and are willing to participate. She added: “The issue of Adverse Childhood Experiences has been a longstanding issue facing our Bermuda community. People in our community are eager to hear whether the data reveals similar results to what the US Ace study revealed.” Family Centre has approached the Inter-Agency Committee for Children and Families, non-profit organisations, and government agencies, asking individuals to send the survey link to members of their network. The Ace survey link is on Family Centre’s website It can also be found on Twitter and Facebook.
2019. March 29. Changes to the island’s health financing are predicted to save millions for the hospital while the Government’s mandated premiums remain unchanged, Kim Wilson, the Minister of Health, announced yesterday. The revamp entails a switch from the hospital’s fee-for-service model, in which all services are separately paid for, to the hospital working within a less costly block grant of $330 million. Ms Wilson said that the ministry had arrived at the figure after discussions since January with Bermuda Hospitals Board. In the event that the hospital broke the $330 million cap, the minister said: “Clearly, the Government is not going to allow the hospital to go under. If there was an event such as some kind of epidemic with increased costs to the hospital, the Government would have to step in.” She said the island was currently saddled with the developed world’s third most expensive health system, with below-average results. This included a national cost of $78 million a year to deal with diabetes and kidney disease alone, which she called “staggering”. Ms Wilson said there would be no increases this year to the public’s standard health insurance premium. Nor would premiums rise for the Health Insurance Plan, or HIP, as well as FutureCare. However, from June 1, the Government will triple the mutual reinsurance fund’s contribution to the standard premium rate. The SPR is the premium for the mandated and basic health package that is part of every insurance policy on the island, and the MRF is embedded within it. Ms Wilson said: “What this means is that whereas currently $101.97 of your standard premium is transferred to the MRF each month, leaving the balance for insurers to pay hospital claims and the other standard benefits, from June 1, $331.97 of the standard premium will be transferred to the MRF, and BHB will receive the bulk of this funding to operate the hospital.” The minister said the changes to BHB’s funding would make “no difference to the ordinary public. Actuarially, it makes no difference to private insurance premiums either. People will pay their insurance premiums just as always. Children, seniors and the indigent will be subsidised as before, and access to hospital services will remain as it is now.” Further consultation is in store, Ms Wilson added, calling it “paramount” that the island develop a better way of paying for healthcare.
2018. March 28. The Bermuda Government’s plans for an overhaul of the healthcare financing system will effectively shift costs from government-backed insurance schemes to private healthcare insurance. The likely result is that employers and the more than 33,000 employees who pay for private-sector insurance will shoulder more of Bermuda’s healthcare cost burden, insurance sources said. Public reports show that government-backed healthcare programmes pay out more in claims than they collect in premiums. For private health insurance, the opposite is true. The Government is planning to pool private and government sources of funding to spread out the cost of heathcare across the entire population. Kim Wilson, the Minister of Health, outlined plans for this fundamental change to healthcare financing in the House of Assembly this month, stating that the plan entails the Bermuda Hospitals Board receiving a $330 million block grant, replacing the “fee-for-service” system. The grant will be capped and the Government claims the change will lead to $20 million of hospital healthcare cost savings. Health insurers are understood to have expressed concerns over the pooling proposals to the Government. One industry source said insurers were informed of the plans only in late January and that the feeling was the financing reform was being rushed through, as more research needed to be carried out on the ramifications for the entire healthcare system, including the impact on employment costs. Employers saw their healthcare obligations increase by 78 per cent in the decade from 2008, research by The Royal Gazette found. Pooling the sources of funding effectively means private insurance will be subsidizing government plans, a source added. An actuarial report for the Bermuda Health Council shows that 48,145 people had health insurance in 2017 — 70 per cent of them covered by private insurers and 30 per cent by government plans. Based on the standard health benefit, the portion of the premium allocated to hospital care coverage, private plans had a loss ratio of 89 per cent, meaning that 89 cents on the dollar were spent on claims and benefits. Government plans had a loss ratio of 143 per cent, meaning premiums fell well short of what was needed to pay claims. On average, private insurers make a profit of about five cents per premium dollar, with about 85 cents going on claims and a further ten cents on operational expenses. The new system will inevitably slash this margin, one source said, meaning health insurers would have to either increase premiums or exit the healthcare business, as continuing to underwrite unprofitable lines of business is not in the interests of shareholders. Detail has not been given, for example, on where the $20 million in cost savings will come from, given that the actual drivers of healthcare cost increases are not being addressed by the reform, the source added. Under the new system, the hospital will no longer need to file claims for treatment of patients, a source said, removing the opportunity for insurers to check the appropriateness of treatments and procedures. This will effectively remove one of the current system’s checks and balances. Claims provide an important source of data on medical trends that help insurers to structure and price coverage to meet changing client needs. Whether the data will be shared across the industry was another source of concern, on which insurers say they have not been given guidance. Ms Wilson is due to give a presentation on healthcare reform to members of the Bermuda Human Resource Association this morning, an event hosted by the Association of Bermuda International Companies at the offices of Axa XL.
2019. March 27. Lahey Hospital in Boston, MA will soon be providing specialist care at the Bermuda Medical Specialities Group clinic on Reid Street. Officials at BMSG announced an agreement with the Massachusetts hospital today. Lahey medical experts will see endocrinology, allergy and immunology, and neurology patients, among others. “The goal at BMSG is to provide access to international level medical services here, on-island in Bermuda while aiming to reduce costs and improve outcomes,” Arlene Basden, BMSG medical director, said. “We started first with Peter Schwartz (cosmetic plastic surgeon), body plethysmography (the gold standard for lung and breathing issues), and are about to launch our non-invasive vascular lab (identification of circulation disease which will lead to reduction in amputations).” Dr Basden said Lahey is no stranger to Bermuda. “Lahey has been a member of the Bermuda healthcare community for over two decades, providing high quality care to the people of Bermuda,” she said. “Our new agreement with Lahey represents our commitment to ensuring that an even wider range of affordable, high quality care is readily available in Bermuda without patients having to incur the costs and stress of traveling overseas.” Richard Nesto, interim CEO, chief medical officer Lahey Health, said: “Lahey Hospital and Medical Centre has chosen to partner with BMSG to help us provide high-quality speciality care on the Island. BMSG’s state of the art facilities provide the ideal setting for the people of Bermuda to receive care from our world-renowned physicians.” BMSG currently provides a range of primary care, specialist, and sub specialist services including cardiology, neurology, rheumatology, pulmonology, endocrinology, asthma, allergy, cosmetic plastic surgery and nutrition. BMSG also provides diagnostic and testing services for each speciality.
2019. March 14. A doctor who wanted to run a walk-in urgent care centre in the heart of Hamilton has claimed a freeze on applications for new services will be “potentially catastrophic”. Dr J. J Soares said a moratorium on requests to provide treatment under the standard health benefit put his almost-completed clinic at risk. Dr Soares added that he was shocked by an e-mail that notified healthcare professionals of the freeze but the health ministry insisted he had been told several times about the process that had to be followed to operate under SHB. Jennifer Attride-Stirling, the health ministry permanent secretary, explained that opening a facility did not guarantee eligibility to have services covered and most clinics operated without SHB approval. The Hamilton Medical Centre in 2016 announced its intention to offer blood testing and diagnostic imaging such as MRI and CT scans under one roof at a new location on Burnaby Street. Dr Soares told The Royal Gazette that he hoped to open the five-floor clinic in the summer. The Bermuda Health Council alerted providers last week to a bar on applications for new services under the basic healthcare package while talks on changes to the healthcare system and its financing were held. Dr Soares claimed he was “blindsided” by the memo. He said: “The moratorium will be potentially catastrophic to the feasibility of the new centre that is at this point approaching completion.” He added: “There was no direct consultation with myself prior to this date about this move by the BHeC. The BHeC has known about my plans for over three years now.” He said the unit would have a walk-in urgent-care clinic open every day from 8am until 10pm, as well as the island’s only open MRI scanner, a CT scanner and facilities for X-ray, mammography, ultrasound and blood tests. Dr Soares said the only service he thought would be covered by SHB — the basic package of benefits that must be included in every health insurance policy — was doctors’ visits. Standard health benefit includes hospital treatment as well as home medical services, non-hospital diagnostic imaging services and palliative, end-of-life home care. Any SHB services that are outside of the hospital are offered by approved providers at a set rate. Dr Soares said: “If we do not have SHB approval then no MRI, CT, ultrasound or X-ray scans will be covered under SHB. What this means is that insurers can decide whether they will pay our facility or not for these scans.” He said lack of approval would mean HIP and FutureCare policyholders were unlikely to have diagnostic imaging covered at the centre. Dr Soares added: “When a patient is seen in our urgent-care centre for an acute illness they should never have to worry whether or not their investigations will be paid for by their insurer. For this reason alone SHB approval is absolutely necessary.” He claimed the freeze on applications would “severely restrict our ability to compete in the marketplace. The viability of the whole project is therefore in jeopardy as a direct result of this moratorium.” A letter from Dr Attride-Stirling to the practitioner dated last September referred to a number of talks over the previous four years. She said she wanted to make sure he understood the distinction between opening up a scanning centre and securing approval to provide those services under SHB. Dr Attride-Stirling wrote: “Significantly, and for clarity, the latter does not preclude the former. However, as you are aware, opening a facility does not automatically give entitlement to SHB eligibility.” The permanent secretary said that “on various occasions” dating back to November 2014 the ministry and Dr Soares discussed SHB coverage and its restrictions. She explained that at a meeting about the doctor’s proposed scanning clinic in August 2016, she and the then health minister pointed out that to be covered by the scheme, the services and facility must be approved by the BHeC. Dr Attride-Stirling said that correspondence from Dr Soares the following month did not suggest he wanted to become an SHB provider. She claimed the BHeC had informed her of similar discussions with the practitioner “over the years”. Dr Attride-Stirling said that most health facilities in Bermuda were not part of the scheme and those services were covered by insurers as supplemental benefits. Dr Soares said yesterday that although conversations with the ministry and BHeC had included explanations about SHB approval, “they never indicated nor did I ever anticipate this sudden announcement of a moratorium being put in place”. He added: “I have always anticipated applying for SHB approval. In fact I did send in an application only to be told that a moratorium was now in place.” Ricky Brathwaite, the acting chief executive of the health council, said: “Once we complete discussions on the redesigned SHB package for 2020 and how much it should cost, we will lift the moratorium to accept applications for those newly defined service areas. New health services can still continue to be added through coverage from our local insurers, despite the moratorium on SHB.”
2019. March 13. A $330 million cash pot is expected to be handed over to the Bermuda Hospitals Board as the Government signaled a new approach to payment for healthcare. The block grant will replace the former “fee for service” method. Kim Wilson, the Minister of Health, told the House of Assembly that it was recognized around the world that the fee for service arrangement was “not the most effective and efficient mechanism”. She was responding to questions from Jeanne Atherden, a One Bermuda Alliance MP, who wanted clarification on a projected $20 million saving in hospital healthcare costs. Ms Wilson said on Monday: “It is correct that the Government is committed, as we indicated in our Throne Speech, to addressing the unsustainable cost of rising healthcare. During negotiations with the Bermuda Hospitals Board we were able to discuss an alternative mechanism for paying for their services.” She added that the change was expected to result in a $20 million saving in healthcare costs this year. Ms Wilson also responded to a question about notice of a moratorium issued recently by the Bermuda Health Council. The memo advised healthcare providers of a freeze on new applications for services under the standard health benefit, which is the most basic package that must be supplied in all insurance policies. She explained that if access to care for essential services was “identified as an issue in the interim”, the BHeC would seek specific applications provided the changes did not affect the standard premium rate. Ms Wilson added: “This moratorium, as has been indicated earlier, is until we have collaborated to determine what will be included in the new standard health benefit package to best address our health needs and we anticipate the new package to be discussed and redesigned over the next few months.” She said the information would be shared with MPs and the public.
2019. March 13. More than $3 million was paid to Bermuda Hospitals Board over 17 months to offset costs incurred by new diagnostic imaging fees, Parliament heard on Monday. Kim Wilson, the Minister of Health, said that from June 1, 2017 to October 31, 2018 that $3.167 million had gone as compensation to BHB. The fee cuts were applied to MRI and CT scanning services in 2017, with payments subsequently made to private providers as well as the hospital. Ms Wilson told the House of Assembly that in the financial year 2017-18 a $780,000 grant was paid to the Brown-Darrell Clinic — a unit in Smith’s owned by former premier Ewart Brown — in relation to diagnostic imaging. Patricia Gordon-Pamplin of the One Bermuda Alliance said that BHB had also adjusted its operating room fees to help the hospital recover some of the revenue lost to the new fees regime.
2019. March 12. The former chief executive of the Bermuda Health Council is to take legal action over her “termination”, she revealed today. Tawanna Wedderburn, who was pushed out of her post last December, said she had asked for judicial review proceedings against David Burt, the Premier, Kim Wilson, the health minister, the BHeC and Alicia Stovell-Washington, the chairwoman of the council. Ms Wedderburn said: “Since this all began I have been bombarded on the streets of Bermuda with well wishes and enquiries about ‘the real story’. My e-mail box is overflowing with encouraging messages from as far away as the Caribbean, Europe and North America. Social media is rife with speculation about the political undertones of the of the case and who is really behind it. All this time, I have been silent. Until now.” The BHeC’s official line at the time was that there had been a “separation of employment”. Ms Wedderburn’s departure from the council led to questions in the House of Assembly a week after it was announced. She added that “there were a series of press releases from the BHeC and the ministry defending their respective positions on the matter” in January. Ms Wedderburn’s husband Livingston later released his account of what had happened and claimed she had been fired without warning. A law firm acting for the BHeC said in January that Ms Wedderburn’s employment was “terminated lawfully by the council in full compliance with section 18(1)(b) of the Employment Act 2000, the Bermuda Health Council Act 2004, and her contract of employment which calls for one-month notice of termination”. It said she was paid her notice and offered six months pay and benefits “in good faith”. Ms Wedderburn said: “I ask everyone in Bermuda to watch the process and take an interest in how these matters unfold as I defer to our judicial system. I extend my sincere gratitude to everyone for their support and encouragement; it has given me the strength, focus and courage to get to this point. May we all benefit from the result.” The Bermuda Health Council in 2017 reduced fees for MRI and CT scans carried out at Bermuda Healthcare Services in Paget and Brown-Darrell Clinic in Smith’s, operated by Ewart Brown, a doctor and former premier. The decision angered Dr Brown, who sent a series of strongly worded e-mails to Ms Wedderburn and other public officials about the cuts, as revealed in a public access to information disclosure by the Ministry of Health last year. He singled out Ms Wedderburn and two other public servants a year ago as he announced the closure of the Brown-Darrell clinic because of the fee cuts. Dr Brown said at a press conference: “Remember these names. Jennifer Attride-Stirling, Permanent Secretary at the Ministry of Health. Tawanna Wedderburn, CEO of the health council, and Ricky Brathwaite, so-called health economist. I want you to remember those names.” The ruling Progressive Labour Party said the slashing of the fees was an “economic vendetta” against Dr Brown by the One Bermuda Alliance government. The PLP administration later handed over $820,000 in public cash to Dr Brown as compensation, with another payout of $420,000 expected.
2019. March 11. Applications for new services under Bermuda’s basic healthcare package have been put on hold while talks to change the scheme take place. Healthcare providers were advised of a moratorium on requests in a memo from the Bermuda Health Council last week as the Government considers ways to reform how the island pays for its treatment. It was hoped discussions among stakeholders would lead to more equal access to care for everyone. The memo said: “The Bermuda Health Council and Ministry of Health are currently reviewing the Standard Health Benefit programme as part of initiatives for system and financing reform. The goal being for all residents to have equitable access to essential care. To ensure that any updates to the SHB programme align to outcomes to be determined through the reform strategy, a moratorium will be placed on all provider-submitted SHB applications for new services until further notice.” Dr. Ricky Brathwaite, acting chief executive of the BHeC and its director of health economics, said last night the missive was issued last Wednesday to let providers know the council was working with other stakeholders on a review of the SHB package. He said: “This redesign is part of initiatives under health system and financing reform. Once we complete discussions on the redesigned SHB package for 2020 and how much it should cost, we will lift the moratorium to accept applications for those newly defined service areas. New health services can still continue to be added through coverage from our local insurers, despite the moratorium on SHB. The majority of non-hospital providers receive their reimbursement in this non-SHB way.” Standard health benefits are the services that must be included in every health insurance policy. They include some hospital and outpatient care, home medical services and diagnostic imaging services. Dr Brathwaite said examples of services that had been added over time included end-of-life palliative care as well as education and training for chronic disease management. The Government is looking at ways to rein in the unsustainable cost of healthcare and a recent briefing note, issued alongside the BHeC, explained that the Ministry of Health planned to move towards a “single-payment mechanism” for the Bermuda Hospitals Board, as opposed to the current “activities-based approach”. It is hoped the move will “put our healthcare system on a more sustainable path and strengthen it for the future”. The note explained that the new style of payment better supported the BHB’s objectives, which were to improve efficiency and achieve the best outcomes and access to care. The approach could result in health system cost savings of about $20 million over the next year, which would be used to minimize SHB premium increases and invest in programmes for prevention and primary care. MPs are expected to debate the 2019-20 health budget today. The House of Assembly is also understood to be covering Bills that amended taxes on land, financial services and the purchase of foreign currency.
 2019. February 13. Bermuda’s
health watchdog has released an information brief as part of a push towards a
value-based healthcare system. A spokeswoman for the Bermuda Health Council
said that alternative payment mechanisms could be used to “reimburse the
delivery of health services, better incentivise collaboration, and move closer
to universal health coverage”. She added that the information provided in the
brief “is part of a larger community conversation around goals for
transitioning our system from a volume-based payment model to one based more on
value”. The spokeswoman said that the price Bermudians are paying for health
insurance had continued to rise. She added: “When paired with the high
incidence of chronic illness and an ageing population with growing healthcare
needs, we are faced with the task of supporting the allocation of resources
necessary to achieve better outcomes, while still improving affordability for
the public.” The spokeswoman said that the healthcare system should be
balanced to ensure that patient care needs are met and that healthcare providers
are “fairly and appropriately” reimbursed. She added: “The right payment
mechanism encourages providers to offer necessary, cost-effective care without
compromising quality, and also ensures that prevention is covered and wellness
is prioritized.” Annabel Fountain, the president of the Bermuda Medical
Doctors Association, said that volume-based reimbursement was sometimes linked
to medically unnecessary work — including lab tests, diagnostic imaging, and
surgeries. She added: “These systems are very expensive and often do not
support preventive care — and can even do more harm.” Dr Fountain said
that value-based systems weighed service outcomes — including patient
satisfaction, reduced hospital readmission rates and wait times, and reduced
complication rates. She added: “Incentives are applied to encourage
cost-effective practices, whilst supporting quality outcomes. Unfortunately, not
all outcomes are based on the quality of the care received.” She explained
that many outcomes are based on other factors including socio-economics,
genetics, and psychological and mental health. “We are concerned that this
might not be acknowledged. However, audit of clinical processes can provide
evidence that clinical guidelines have been followed, supporting reimbursement
even if the outcome is not optimal.” The brief can be seen on the Bermuda
Health Council website.
2019. February 13. Bermuda’s
health watchdog has released an information brief as part of a push towards a
value-based healthcare system. A spokeswoman for the Bermuda Health Council
said that alternative payment mechanisms could be used to “reimburse the
delivery of health services, better incentivise collaboration, and move closer
to universal health coverage”. She added that the information provided in the
brief “is part of a larger community conversation around goals for
transitioning our system from a volume-based payment model to one based more on
value”. The spokeswoman said that the price Bermudians are paying for health
insurance had continued to rise. She added: “When paired with the high
incidence of chronic illness and an ageing population with growing healthcare
needs, we are faced with the task of supporting the allocation of resources
necessary to achieve better outcomes, while still improving affordability for
the public.” The spokeswoman said that the healthcare system should be
balanced to ensure that patient care needs are met and that healthcare providers
are “fairly and appropriately” reimbursed. She added: “The right payment
mechanism encourages providers to offer necessary, cost-effective care without
compromising quality, and also ensures that prevention is covered and wellness
is prioritized.” Annabel Fountain, the president of the Bermuda Medical
Doctors Association, said that volume-based reimbursement was sometimes linked
to medically unnecessary work — including lab tests, diagnostic imaging, and
surgeries. She added: “These systems are very expensive and often do not
support preventive care — and can even do more harm.” Dr Fountain said
that value-based systems weighed service outcomes — including patient
satisfaction, reduced hospital readmission rates and wait times, and reduced
complication rates. She added: “Incentives are applied to encourage
cost-effective practices, whilst supporting quality outcomes. Unfortunately, not
all outcomes are based on the quality of the care received.” She explained
that many outcomes are based on other factors including socio-economics,
genetics, and psychological and mental health. “We are concerned that this
might not be acknowledged. However, audit of clinical processes can provide
evidence that clinical guidelines have been followed, supporting reimbursement
even if the outcome is not optimal.” The brief can be seen on the Bermuda
Health Council website.
2019. February 8. The acting chief executive of Bermuda’s healthcare watchdog set up a company with a top executive from the US-based Lahey Clinic but “immediately terminated” the arrangement because of a potential conflict of interest, it has been revealed. Ricky Brathwaite, the former director of health economics at the Bermuda Health Council, incorporated Dyenic Group International with Linda Moulton, the former chief executive of Lahey’s executive and international health programmes, in Massachusetts in May 2016. Alicia Stovell-Washington, the health council chairwoman, said Dr Brathwaite and Ms Moulton, who met in Bermuda, ended their business relationship in June that year after the BHeC decided there were “potential perceived conflicts with Ms Moulton’s then employer, Lahey International”. She added: “Per recent statements, the health council would like to make mention that Dr Ricky Brathwaite states that he has never engaged in relationships with any aspect of the Lahey business or Dr Ewart Brown outside of his official capacity at the council.” Dr Stovell-Washington was speaking after a report on ZBM News on Wednesday questioned why a “high-ranking officer of the island’s health services watchdog partnered with a person formerly responsible for attracting foreign business” to Lahey, a hospital in Massachusetts. The report included a March 2016 photograph of Ms Moulton presenting a plaque from Lahey to Dr Brown, the former premier, for starting a programme that brought specialists from Lahey to treat patients in Bermuda. Dr Brathwaite joined Bermuda Health Council as programme manager for health economics in 2014 and later became director of health economics. He was made acting CEO of the regulatory body in December, after former chief executive Tawanna Wedderburn was fired. When he met Ms Moulton, she was responsible for helping Lahey to develop markets to provide medical care to patients outside of the United States. Ms Moulton said last night: “An entity was formed in 2016. There was a concept of shared faith, through the Seventh-day Adventist church, and a commitment to service, which led to an idea of helping underserved communities. “Once we realised that it might lead to confusion because of our professional roles, we handed it off. The entity still exists, as you can see from the filings.” Ms Moulton added: “I left Lahey to take my current role working with an organisation that provides healthcare and education in East Africa. It’s really that simple and was formed with good intentions.” Lahey already had a relationship with Bermuda and sent its specialists to the island as part of the programme announced by Dr Brown in 2007, when he was premier in the Progressive Labour Party government. Dr Brown’s own business relationship with Lahey, involving his two medical clinics, would later come under the spotlight when the former One Bermuda Alliance government sued the hospital for allegedly conspiring with him to carry out a “corrupt” scheme “at the expense of the Bermudian government and people”. The lawsuit, filed in the United States, claimed Dr Brown used his position as a government minister to promote Lahey’s interests in Bermuda, and the hospital paid him “bribes disguised as consulting fees” to do so. The hospital and Dr Brown denied the accusations and the case was dismissed by a judge in March last year. Dr Stovell-Washington said the health council was made aware in May 2016 that Dr Brathwaite had incorporated Dyenic, which stands for Dynamic Youth Envisioning New Ideas for Change. She added: “This initiative was one that Dr Brathwaite had begun in 2001 while studying at the University of Maryland. Ms Linda Moulton, whom Dr Brathwaite met in Bermuda, then partnered with him on an expanded initiative to provide support to vulnerable youth and underserved communities in the United States and other African diaspora countries outside of Bermuda.” Dr Stovell-Washington added: “The health council board discussed the potential conflict of interest of the arrangement in June 2016, which resulted in the decision for Dr Brathwaite not to engage further due to the potential perceived conflicts with Ms Moulton’s then employer, Lahey International.” She said: “Dr Brathwaite still volunteers as a mentor and provides support to programmes for youth here in Bermuda and in the United States.” Dyenic’s certificate of incorporation with the corporations division of the Commonwealth of Massachusetts said that it provided “strategic consulting to hospitals and healthcare systems”. Ms Moulton filed its last annual report in April last year and Dr Brathwaite was still listed as having an interest. Dr Brathwaite told The Royal Gazette yesterday: “There was never any operations of any business that took place.” A spokesman for the Lahey clinic said that “employees are required to proactively disclose any potential conflict of interest to Lahey’s health compliance department”. He added: “Linda Moulton is no longer an employee of Lahey Hospital & Medical Centre or any business unit within the Lahey health system.” A Ministry of Health spokeswoman said: “The Bermuda Health Council recruits its own employees — the Ministry of Health is not involved in its hiring. The ministry was made aware of a business partnership, which began years after Dr Brathwaite began employment at the health council. The matter was addressed at the time by the Bermuda Health Council.” The health council was set up to regulate private health service providers, ensure the provision of essential health services and to promote good health.
2019. February 7. A premiums hike in the government employee’s health insurance scheme could hit seniors on fixed incomes, campaigners for the elderly have warned. Now the Bermuda Senior Islanders’ Centre has urged older Bermudians to push politicians to force down health insurance costs in the wake of a rates rise in the scheme for government workers. Contributions from public sector staff and retirees increased by more than 5 per cent last week, which increased their monthly charge to more than $400. Rates for non-employed spouses and dependents were also affected by the hikes. Fred Hassell, the director of Bermuda Senior Islanders’ Centre, said the organisation was worried about the impact on people with limited means. He said: “We’re concerned about seniors affected by increases in the cost of living while on determined incomes. We feel for those who can’t absorb the increase and are forced to use their meager income to cover the additional increase in premiums. Our advice for fellow seniors is to keep up the pressure on MPs to do more to get the cost of health insurance in the reach of all citizens.” Government Employees Health Insurance rates went up last Friday from $381.85 to $402.51 a month for each worker or retiree and the cost for non-employed spouses rose by nearly $31 to $603.77 — a 5.4 per cent increase. The Ministry of Finance claimed the increases struck “the right balance” between availability and cost of the coverage. The change came after seniors and other recipients of Contributory Pension Fund benefits heard last December payments would be boosted by 1.4 per cent, with the rise backdated to August. Claudette Fleming, the executive director of Age Concern Bermuda, highlighted that several problems needed to be tackled as the population ages. A population projections report predicted that one in four residents will be aged 65 or over by 2026. Dr Fleming said: “The state of the GEHI programme is indicative of the severe impact of the demographics of our time. A delicate balance must be exercised to keep the plan solvent while at the same time not causing financial harm to those who may need the coverage the most, especially for retirees. This demographic scenario will play itself out many times over on many different fronts as the Bermuda population ages rapidly. The oversight body of GEHI have a responsibility to ensure that it is available to current employees and retirees. Policyholders can inquire and make a judgment call on how well GEHI is being managed.” Dr Fleming added: “In the meantime however, demographics are not on our side when it comes to insurance. FutureCare remains an option for those seniors who cannot afford increased premiums. However, even FutureCare will have its limits at some point. We encourage seniors to think about options, albeit these options are extremely limited.” The GEHI scheme covers all government pensioners, employees and their dependents, The Government’s website said it was a programme that provided “premium healthcare at fair rates” with swift claims processing. A Ministry of Finance spokeswoman said the increases came after an actuarial report on the scheme. She added: “This premium adjustment will help to ensure that the GEHI plan remains viable in the long term and meets the primary objective for which it was established, to provide affordable health insurance benefits for government employees, retired government employees, and their enrolled dependents. The ministry has considered the impact that these premium increases will have on the members of the plan and believes this adjustment strikes the right balance between social and fiscal responsibility.”
2019. January 24. A $20 million increase in health spending failed to deliver a healthier Bermuda, it was feared yesterday. The 2018 National Health Accounts Report showed the total public and private expenditure neared $723 million in 2016-17. Bermuda was third behind only the United States and Switzerland in a list of Organisation for Economic Co-operation and Development countries when compared by health spending as a percentage of GDP. However, the $7,220 outlay per person resulted in a life expectancy at birth of 81.3 — lower than several other countries that spent less. The report noted: “Bermuda falls below the trend for health expenditure and life expectancy which suggests we are spending more without achieving greater health outcomes. “This is further supported when we compare Bermuda to other jurisdictions of similar affluence [per capita GDP] such as Norway, where health expenditure is less but life expectancy is higher. Switzerland, also of similar affluence, has a higher per capita health expenditure but also has a longer life expectancy.” Data published on the BHeC website showed the OECD average spend for the fiscal year ending March 31, 2017, was $3,996 per person and average life expectancy was 80.5. Expenditure per head in Norway was found to be $6,647 but, at birth, people there can expect to live to 82.4. In Switzerland, the health cost for each person was $7,919 but their life expectancy was 83. The report found Bermuda’s health spend was 11.5 per cent as a share of its GDP, behind only Switzerland at 12.4 per cent and the US at 17.2 per cent. The OECD average was 9.08 per cent. Tiara Carlington, a BHeC policy analyst for data and research, said yesterday: “This report provides us with a basis for looking at the bigger picture of how policy decisions can affect our health system’s success. Looking at the findings of these reports over time, it is clear that we have to move away from the expectation that more expensive care means better care. Instead, we need to be more sensible about how we spend and align our spending with our system’s long-term goals — once we make that change we can begin to expect more.” The National Health Accounts Report identified trends in the health system finances and looked at how the island compared to other jurisdictions. The BHeC said in a statement: “As has been the general year-over-year trajectory, total health financing and expenditure increased. This increase of $20 million in spending represents a 2.26 per cent uptick, which supports what is expected as the population ages and our communities learn more effective ways to prevent and manage the existing burden of chronic disease.” The BHeC said there was a small change in the typical distribution of financing, with a drop in health insurance as a portion of funds overall and a rise in out-of-pocket payments. It added: “To better understand the cause of this shift, and its impact on the sustainability of the health system and individuals’ access to care, we are moving towards greater enforcement of the Claims Regulations’ legislation. The existing legislative requirement supports provider reporting of their full charges for health products and services including the insurance covered portion and the total out-of-pocket co-payment.” Ricky Brathwaite, the BHeC’s acting chief executive and director of health economics, said: “This report also demonstrates an important opportunity for Bermuda’s overall financial flexibility. We must seek to create initiatives to encourage economic growth while simultaneously working diligently on reducing health expenditure.” Kim Wilson, the health minister, welcomed the report yesterday and described it as “essential data and analysis. The trends reported are helping to inform policy decisions about how to address healthcare costs for the public and employers, and it provides vital insights into the health financing problems to guide and inform solutions.” Ms Wilson said the ministry continued to assess feedback from stakeholders who reviewed two health insurance models last year after they were first mooted in 2012. She added: “We will be in a position to share next steps in the coming months.” Patricia Gordon-Pamplin, the One Bermuda Alliance’s shadow health minister, said yesterday: “This government can talk all it likes about different insurance systems, but unless, or until, it is prepared to take some tough decisions, until there is better control of what is used and how often, until we are able to get more people on the island to spread the cost of healthcare, the reality is that costs will just continue to rise. It should really alarm people that healthcare costs for a community the size of a small US town are forecast to reach $1 billion.”
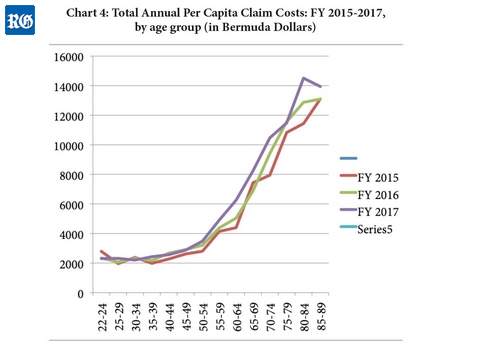 2018. December 17. Without
effective regulation of medical-services providers and moves to cover the
sizeable minority who have no health insurance, healthcare costs are likely to
keep spiraling. That is the view of executives at BF&M Ltd, a major health
insurer on the island. They said the failure to address the drivers of high
costs, combined with the ageing population and a shrinking working-age
population paying into the system amounted to a “ticking time bomb”. John
Wight, the insurer’s chief executive officer, and Michelle Jackson, senior
vice-president, group lines, health and life, said in an interview the Bermuda
Government’s proposals to reform healthcare financing was “the wrong
starting point” for the changes needed. Government’s plans to increase
cross-subsidization of costs from the healthy to the sick amounted to
effectively shifting costs around, they said. Mr Wight said that change was
needed “to address the high cost of healthcare, rather than who pays for
healthcare”. He urged employers to be more outspoken about the financing
reform plan. “We need to have more employers weigh in on what this initiative
means to them,” Mr Wight said. “They are going to be the ones bearing the
cost of it. There is a better direction for Bermuda to take and that’s to
address the drivers of increasing healthcare costs.” Ms Jackson said one such
driver was the growing number of uninsured people. “More than 8 per cent of
the population is not employed and without healthcare coverage,” Ms Jackson
said. “They are not getting regular medical treatment and some are turning up
at the emergency room with long-term care issues.” The use of the hospital as
a primary source of care by the uninsured was hugely expensive for the system as
a whole, she added, and drove up premiums. "We have to address the
situation that more and more people are finding themselves in,” Ms Jackson
said. “Many people are hurting and something has to change.” More long-term
care solutions were badly needed, particularly with Bermuda’s demographic
pressures, she added. Government population projections estimate that 10.8 per
cent of the population will be over 75 by 2026, when one in four will be over
65. Meanwhile, Ms Jackson said the island had lost about 6,500 people since
2010, many of them healthy, working people aged between 25 and 55, who were
paying more into the system than they were taking out, thus helping to subsidies
older people who used more health services. “We have not got the long-term
care services we need,” Ms Jackson said. “We have not planned for the number
of people who will need these services.” Mr Wight said it had been 48 years
since the healthcare system had seen serious reform with the Bermuda Hospitals
Board Act 1970 and the Health Insurance Act of the same year. The system was
overdue for change, he said. “We insurers are regulated and the
medical-services providers should be regulated as well,” Mr Wight said.
“Without regulation, it’s difficult to see how we are going to be able to
contain costs.” The Fiscal Responsibility Panel report, released this month,
backs up Mr Wight’s view. It states: “The private medical care sector in
Bermuda is largely unregulated, raising concerns about both the cost and quality
of the care provided, of diagnostic testing and of pharmaceutical products.
Further efforts are needed to strengthen the regulation of private sector
providers (including their use of health technology) as a means to reduce
duplication that adversely impacts healthcare costs and exposes patients to
unnecessary risk.” The economic experts who penned the report said “an
appropriate regulatory infrastructure with enforcement resources remains a
necessary element of any strategy for cost containment in Bermuda’s healthcare
sector”. The report also warns: “The island’s costly healthcare system
risks overwhelming the budget and the whole economy as the population becomes
increasingly elderly and frailer, with more and more requiring long-term
care.” The panel goes on to recommend:
2018. December 17. Without
effective regulation of medical-services providers and moves to cover the
sizeable minority who have no health insurance, healthcare costs are likely to
keep spiraling. That is the view of executives at BF&M Ltd, a major health
insurer on the island. They said the failure to address the drivers of high
costs, combined with the ageing population and a shrinking working-age
population paying into the system amounted to a “ticking time bomb”. John
Wight, the insurer’s chief executive officer, and Michelle Jackson, senior
vice-president, group lines, health and life, said in an interview the Bermuda
Government’s proposals to reform healthcare financing was “the wrong
starting point” for the changes needed. Government’s plans to increase
cross-subsidization of costs from the healthy to the sick amounted to
effectively shifting costs around, they said. Mr Wight said that change was
needed “to address the high cost of healthcare, rather than who pays for
healthcare”. He urged employers to be more outspoken about the financing
reform plan. “We need to have more employers weigh in on what this initiative
means to them,” Mr Wight said. “They are going to be the ones bearing the
cost of it. There is a better direction for Bermuda to take and that’s to
address the drivers of increasing healthcare costs.” Ms Jackson said one such
driver was the growing number of uninsured people. “More than 8 per cent of
the population is not employed and without healthcare coverage,” Ms Jackson
said. “They are not getting regular medical treatment and some are turning up
at the emergency room with long-term care issues.” The use of the hospital as
a primary source of care by the uninsured was hugely expensive for the system as
a whole, she added, and drove up premiums. "We have to address the
situation that more and more people are finding themselves in,” Ms Jackson
said. “Many people are hurting and something has to change.” More long-term
care solutions were badly needed, particularly with Bermuda’s demographic
pressures, she added. Government population projections estimate that 10.8 per
cent of the population will be over 75 by 2026, when one in four will be over
65. Meanwhile, Ms Jackson said the island had lost about 6,500 people since
2010, many of them healthy, working people aged between 25 and 55, who were
paying more into the system than they were taking out, thus helping to subsidies
older people who used more health services. “We have not got the long-term
care services we need,” Ms Jackson said. “We have not planned for the number
of people who will need these services.” Mr Wight said it had been 48 years
since the healthcare system had seen serious reform with the Bermuda Hospitals
Board Act 1970 and the Health Insurance Act of the same year. The system was
overdue for change, he said. “We insurers are regulated and the
medical-services providers should be regulated as well,” Mr Wight said.
“Without regulation, it’s difficult to see how we are going to be able to
contain costs.” The Fiscal Responsibility Panel report, released this month,
backs up Mr Wight’s view. It states: “The private medical care sector in
Bermuda is largely unregulated, raising concerns about both the cost and quality
of the care provided, of diagnostic testing and of pharmaceutical products.
Further efforts are needed to strengthen the regulation of private sector
providers (including their use of health technology) as a means to reduce
duplication that adversely impacts healthcare costs and exposes patients to
unnecessary risk.” The economic experts who penned the report said “an
appropriate regulatory infrastructure with enforcement resources remains a
necessary element of any strategy for cost containment in Bermuda’s healthcare
sector”. The report also warns: “The island’s costly healthcare system
risks overwhelming the budget and the whole economy as the population becomes
increasingly elderly and frailer, with more and more requiring long-term
care.” The panel goes on to recommend:
The report added that the Ministry of Health’s recent adjustment of the Bermuda Hospitals Board fees for different services based on an international standard was “an important first step in the direction of cost control”. Chronic diseases, often a result of lifestyle choices, are a huge drain on the system. On the plus side, Mr Wight said that many of his company’s clients had introduced wellness programmes and were seeing premiums and sick days fall as a result. Ms Jackson added that awareness was growing. “It’s not terribly complicated, what we need to do, and there’s some really good work being done by different organisations to get the word out,” she said. The government consultation on health financing reform, which included representatives of insurers, the medical profession, employers and unions, found support for deeper reforms. According to brief minutes of a stakeholder consultation group meeting on October 17, published on the government website, those present noted that “quality, outcomes and costs to consumers were not directly addressed in a change in financing structure”. At another meeting on October 31, there was support for means-tested subsidy reform, expansion to a prevention-based system shifting away from fee-for-service, a focus on providing universal coverage and provisions for chronic disease management. The minutes continued: “There is definitely an urgency for change but also a desire that that changes are completed strategically and in the most effective order.” Healthcare cost inflation in Bermuda is estimated at around 6.5 per cent annually, roughly five percentage points higher than overall inflation, as measured by the Consumer Price Index. "So what will health insurance premiums look like in five years’ time if there is no reform of the system? We’ve had some actuarial studies done and all I can say is that it doesn’t look pretty,” Ms Jackson said.
2018. December 15. The departure of a health watchdog’s chief executive should raise red flags, the shadow health minister said yesterday. Patricia Gordon-Pamplin said that the “removal” of Tawanna Wedderburn from the Bermuda Health Council was done “with no proper explanation”. Ms Gordon-Pamplin told the House of Assembly: “We have had only the vaguest of statements as to why she has left her post, which is extremely unsatisfactory.” She asked Kim Wilson, the Minister of Health, to provide a “fulsome public explanation”. Ms Gordon-Pamplin said: “Mr and Mrs Bermuda deserve to know why someone in such a key position has suddenly left her post.” It was announced earlier this month that Ms Wedderburn had left the BHeC. The council confirmed “the separation of employment” between Ms Wedderburn and the organisation on December 7. The BHeC thanked Ms Wedderburn for her service and wished her “every success in her future endeavors” but gave no reason for her departure. It added that it would “soon” announce the appointment of an acting chief executive and declined to comment further. A government spokeswoman said yesterday the health ministry was grateful to Ms Wedderburn for her “passionate commitment to help patients and the public” while at the BHeC. She added: “However, it would be wholly inappropriate for the ministry to comment publicly on matters pertaining to any individual’s employment.” Ms Gordon-Pamplin added that the Government had to “get to grips” with increases in healthcare costs, including “the overutilisation of some services, as well as issues like obesity and diabetes”. She warned: “In failing to do that, the Minister of Health is just passing the buck down to future generations.” Ms Gordon-Pamplin said that Ms Wedderburn had been “acutely aware of the need to control the costs of services in order to help keep the cost of insurance down”. She added that healthcare costs in Bermuda were predicted to hit $1 billion in five years. Ms Gordon-Pamplin added: “For a population of a little over 60,000, that is just unsustainable.” Ewart Brown, a former premier, blamed the BHeC and its fee cuts for the closure of his CT scanner unit at his Brown-Darrell Clinic in Smith’s. Dr Brown accused the council last January of a political “vendetta” against him and singled out several members, including Ms Wedderburn. The decision, taken under the previous One Bermuda Alliance Government, was later moderated by its successor, the Progressive Labour Party administration. The Bermuda Hospitals Board and private services such as Dr Brown’s were hit by the fee cuts, which later resulted in payouts from the Government. Ms Wilson later said payments to Dr Brown’s two practices were likely to exceed $1.2 million. She told Parliament last month that BHB had been compensated by about $1.86 million up to March 2018. Increased fees for diagnostic imaging came into force at the start of last month. The Brown-Darrell Clinic announced this week that it would restart high-tech CT scans on Monday.
2018. December 14. A clinic run by Ewart Brown, a former premier, is to restart hi-tech CT scans almost a year after the plug was pulled on the computerized imaging service. The Brown-Darrell Clinic in Smith’s will bring back the scanning service on Monday. Dr Brown signaled in September that the scans would resume. Dr Brown said yesterday: “We delayed the reopening until we could find a vastly proficient technologist who is experienced in all aspects of CT scanning including special cardiac studies.” The service was shut down in January after major fee cuts for scans were introduced by the former One Bermuda Alliance government, a position later moderated by its Progressive Labour Party successor. Increased fees for diagnostic imaging came into force at the start of last month. Dr Brown said that the Lahey Hospital and Medical Centre in Massachusetts would continue to interpret scans carried out in Bermuda. The Bermuda Hospitals Board and private services such as Dr Brown’s were affected by the fee cuts, which resulted in payouts from the Bermuda Government. Kim Wilson, the Minister of Health, later said payments to Dr Brown’s two practices were likely to exceed $1.2 million. Ms Wilson told Parliament last month that BHB had been compensated by about $1.86 million up to March 2018. A spokeswoman for the Ministry of Health said last night that the fee rates update marked the conclusion of the Government’s compensation commitments.
2018. December 7. Tawanna Wedderburn has left the Bermuda Health Council, where she had served as chief executive, the BHeC announced this afternoon. According to a statement, the health watchdog is soon to announce the interim appointment of an acting CEO until a new chief executive can be put in place. The BHeC thanked Ms Wedderburn for her service since 2015.
2018. December 4. A special reserve fund could help to balance the risk in one of two “transformational” health insurance options being considered by the Government. The reserve would allow funds to flow between insurers with relatively healthy policyholders, who take little out of the system, and those whose members put greater demand on services. In the other option, a single body would manage standard package payments for everyone in Bermuda and only supplementary benefits would be covered by private companies. Kim Wilson, the health minister, outlined the schemes after a Throne Speech pledge to develop a national plan that will put all island residents into either one of two health insurance pools. She told The Royal Gazette that a change was needed to balance the provision of a good standard of healthcare at a reasonable cost. Ms Wilson said: “One is we need to reduce premiums. Two is we need to ensure that everyone in Bermuda has affordable insurance coverage. Three we need to improve basic coverage to help promote health; and then, finally, of equal importance, is to contain costs. At this point we spend over $700 million a year on healthcare. Obviously, that’s not sustainable. In order to draw that in, we need to find a better way in which we are collecting the money and how that money is spent with respect to the provision of healthcare; that’s where health-financing reform comes in.” Better use of resources was one of 14 goals listed in the Bermuda Health Strategy 2014-2019, which also included regulation of clinical care standards and the encouragement of healthy lifestyles. Ms Wilson explained that thousands of health insurance pools are operated in Bermuda. She said the smallest groups would feel the effects of major demands made by their policyholders, for example in the case of a catastrophic injury or illness, more than if they were in larger groups. Ms Wilson added: “We’re looking at pooling all 65,000 people; all of the population will be pooled in either one of two pools so that we’re spreading the risk.” She added: “We would also be looking at introducing a benefits package that would include things like hospitalization, medication, long-term care, preventive care ... that particular benefits package would be costed out and we do believe it would be more economical than what is the current position.” The minister added that a bipartisan committee carried out “extensive work” in 2012 and came up with two financing options. One was the unified model, where a single insurer provides the standard health benefit, a basic package expected to include medication as well as long-term and preventive care, and distributed payments to providers. This is a similar approach to Canada’s and would mean private insurers offered supplemental benefits. Ms Wilson said there were three options to manage the basic package payments — a private insurer, quango or, maybe the “least desirable”, a government department. She explained: “If the decision was to go with a private insurer there would have to be a request for proposals and a very comprehensive procurement and competition to decide who was going to get such a large package, because we would be talking about hundreds of millions of dollars.” The second proposal is a dual model, which would include a large public insurer covering standard benefits and ensuring provision for government-led schemes such as the Health Insurance Plan and FutureCare. Private insurers could also sell the standard health benefit as well as their supplementary coverage. Several European countries, including Switzerland, manage healthcare financing under similar schemes. Ms Wilson added: “The difference here between this and what happens now is that currently insurers have to include standard health benefit in any package by law but they don’t actually have to insure anyone, so they can deny you for pre-existing conditions, they can deny you if you’re over 75, which they all do universally, so they have flexibility on what risk they take on. So if you’re bad risk, they don’t accept you. In the dual model, that wouldn’t be allowed, you would have to take whoever came to you at any time, in whatever state they’re in.” Ms Wilson said a “very significant” aspect of the dual system would be the inclusion of a “risk equalizer” that acts like a funds reserve or cash pot. She explained: “If any insurer ends up with a very healthy pool and they ended up making money off SHB — if they paid less in claims than the premium they collected — then they would have to give some money back to the risk equalizer, so that the other insurer that wound up with very sick people — spending more than they collected — then they would have to get the money back from the risk equalizer.” A consultation group that included employers, unions, insurers and medical representatives recently reviewed the 2012 recommendations and submitted responses. Ms Wilson started to look over the submissions last week and said she planned to make recommendations to Cabinet this month so that ministers can decide which of the two options should be chosen. She added more work and further public consultation will follow, with town hall-style information meetings possibly “in the first quarter” of next year. Ms Wilson said a new system could not come soon enough. But she added that the effects of a change would be seen by 2020. Ms Wilson said: “This is a huge process and a huge shift from how we’ve been doing it heretofore, so I have to learn to be patient. This is truly transformational.”
2018. December 3. A new education campaign designed to boost knowledge about asthma was sparked by the tragic death of a young boy in Britain. Open Airways, an island asthma charity, is offering the Support Children’s Health-Asthma online course. The George Coller Memorial Fund and Education for Health UK created the programme. It was launched by Kim Douglas in 2000 after the death of her son, George Coller, who was 3 and died in his sleep from asthma in 1996. A spokeswoman for Open Airways said that 20 per cent of children and 10 per cent of adults in Bermuda had asthma. She added: “Many of these children and adults have uncontrolled asthma, which results in asthma attacks and potentially asthma deaths.” The spokeswoman said it was estimated that more than 1,000 people died globally from asthma each day. She added: “The majority of these are children of young adults and, tragically, most of these deaths were preventable.” The online module covers areas such as how to recognize an asthma attack and what to do if an attack strikes. The free course, aimed at people who work with or have children with asthma, takes about an hour to complete. A certificate can be printed after the course work is completed. The course is offered in a link-up with insurance firms Argus Group and BF&M. For more information, visit openairways.com.
2018. November 30. A pilot program designed to beam diagnostic imaging results direct to doctors and patients has been launched by the Bermuda Hospitals Board. Renée Butterfield, the manager of diagnostic imaging at King Edward VII Memorial Hospital, said the scheme was “all about ease of access”. She explained the Picture Archiving Communication System would mean an end to the use of fax machines or CDs to send doctors CT scans, X-rays and mammography results. The scheme also means patients could get unprecedented access to their scans. The electronic scheme was adopted a year ago and is now accessible throughout King Edward VII Memorial Hospital. Pacs has been popular with orthopaedic doctors and some physicians, but Ms Butterfield said the hospital wanted to see more private practices take it up. Ms Butterfield added: “The beautiful thing about it is you not only have access to the image, you can also access the report. We also have a strong support team accessible 24 hours a day.” Two portals are being piloted at KEMH — one for physicians, and another for patients. Ms Butterfield said: “We’ve put together a list of physicians who will test it.” Tracy Sampson, a senior X-ray technician, said the hospital was testing the system on “various physicians that request it” and hoped to recruit more. She added: “All they have to do is communicate with us and provide feedback.” The patient access portal is expected to go live early next year. Ms Butterfield added that the turnaround time for reports had been cut. She said: “Nothing is perfect, but we’re on our way.” November 8 marked the International Day of Radiology and Bermuda’s imaging services staff used the week to highlight their work.
2018. November 27. Businesses affected by the new tax on sugary products will not qualify for compensation the way providers of high-tech medical scans did, MPs have been told. Kim Wilson, the health minister, said that businesses had been given advance notice of the new tax, but those that offered diagnostic imaging had been hit “without consultation and warning”. The news came as the minister gave a breakdown in the House of Assembly on payments to Ewart Brown, a former premier and a doctor, and the Bermuda Hospitals Board, after fees for MRI and CT scans were slashed last year. Ms Wilson said Dr Brown’s Bermuda Healthcare Services in Paget was given $680,966 between December last year and May. The Brown-Darrell Clinic in Smith’s, Dr Brown’s other practice, got a total of $139,151 in five payments over the same period. The Bermuda Hospitals Board was compensated to the tune of $1.863 million in nine payments from December 2017 to March 2018. The details were released in response to parliamentary questions on Friday from Patricia Gordon-Pamplin, the shadow health minister. Payments were calculated by the Bermuda Health Council, using information from the providers and details from insurance companies. Ms Wilson said the Government had drawn a line on payments to businesses hit by the sugar tax, which came into effect on October 1. She added: “There was public consultation before the decision was made and businesses had time to prepare. This does not compare to the fees that were imposed without warning or consultation on diagnostic imaging.” Ms Gordon-Pamplin told the House that information on diagnostic imaging changes had been provided by officials who were “intimately involved at the time”. Dr Brown, who shut down the CT scanning unit at the Brown Darrell Clinic earlier this year, has maintained that the scanning fees were cut without any consultation.
2018. November 27. Legal changes to bring midwives under the same umbrella as nurses has passed in the House of Assembly. Kim Wilson, the Minister of Health, told MPs that the old legislation covering midwives “contained an outdated regulatory framework” that resulted in “a limited scope of practice and regulatory oversight”. She added: “The ministry remains in ongoing consultations with registered midwives and other stakeholders for a phased approach to enhance safety and quality of care for women and babies, as well as address choice and potential cost savings for the health system.” The Nursing Amendment Act 2018 merged legislation for midwives with the Nursing Act 1997 and repealed the Midwives Act 1949. It also shifted the regulatory authority for midwives from the Bermuda Medical Council to the Bermuda Nursing and Midwifery Council. The new Act was passed without objection on Friday night. Tinée Furbert, a Progressive Labour Party backbencher, said that the changes took “an ancient piece of legislation and now brought it up to date”. Patricia Gordon-Pamplin, Shadow Minister of Home Affairs, said that any new legislation must “ensure that every birth is safe, that every baby is safe, and that every mother is safe.” She said that merging the two professions together was “a positive thing” for efficiency and that the One Bermuda Alliance supported the legislation “in principle”. Ms Gordon-Pamplin added: “We just want to know that whatever we are doing, it continues to enhance the safety, the security, the comfort and the medical attention that is necessary to provide for a good outcome for both mother and child.” Susan Jackson, shadow health minister, said that she hoped Bermudian youngsters would consider midwifery as a career path. She added: “Certainly, we are all aware of the costs of going into the hospital and having a child.” Ms Jackson said that further steps should be taken to improve midwifery qualifications. She added that she hoped Bermuda continued to “foster this profession as a means of providing an alternative to mothers who are looking to have their children outside of the hospital”. Ms Wilson said it “would have been nice to hear” from a male MP during the debate. However, she added that she thanked her colleagues for the cross-party support.
2018. November 21. A three-pronged threat from chronic health problems and an ageing population could lead to a leap in the number of Alzheimer’s disease sufferers, a British expert warned yesterday. Tim Forester-Morgan said diabetes, heart disease and an ageing population were all risk factors that contribute to the condition. He added: “The prevalence of diabetes on the island is the second highest in the world and the World Health Organisation has highlighted that this is a significant risk factor for Alzheimer’s disease. Bermuda has a high rate of heart disease, which has also been shown to increase the possibility of the disease. Add to this the country’s ageing population and you have a combination of factors that together suggest a very significant risk that the numbers of people who could be living with dementia in Bermuda could increase quite sharply over the next few years. Mr Forester-Morgan and Sarah Mould, directors of the British-based Dementia Training Company, have been on the island for the past six days to highlight the latest research and advice to caregivers and public service teams. They were invited by Elizabeth Stewart, founder and president of Action on Alzheimer’s and Dementia, which is working on a national strategy to provide guidelines for people and organisations involved with Alzheimer’s patients. It is the fourth time the pair have visited and both said awareness in the community had increased over the years. Bermuda Alzheimer’s and Memory Services said about 2,000 people on the island have dementia, which causes a deterioration in memory, thinking, behavior and the ability to perform everyday tasks. The Government said yesterday that the actual number of sufferers was not known but “informal estimates” suggested it was about 1,000. Alzheimer’s is the most common form of dementia and the WHO has said it may make up between 60 and 70 per cent of cases. A 2011 comparison of Organisation for Economic Co-operation and Development countries showed Bermuda’s diabetes prevalence was more than ten per cent — the second highest in the survey. The 2017 Health in Review report showed cardiovascular disease was the biggest killer in Bermuda and accounted for a third of all deaths in recent years. Ms Mould said the connections had been made between these conditions and Alzheimer’s. She added: “It now feels like people are hearing the message. Certainly the GPs, I think, were quite shocked by some of the information we provided but also committed to doing something about it.” The pair have undertaken a programme of events, including training with police and fire crews, nursing students, family caregivers and charities. Mr Forester-Morgan and Ms Mould joined Ms Stewart for a meeting with representatives from the Ministry of Health as well as the Ageing and Disabilities Services. Ms Stewart hoped a national strategy could be developed in line with a Pan-American Health Organisation regional plan of action, published in 2015. The document committed countries to creating plans that include risk reduction through public health programmes, better training for healthcare professionals and ensuring everyone affected by dementia received the same opportunities for care and support. Ms Mould said people in Bermuda had asked her what needed to be done next. She added: “People are recognizing we need more specialized services, perhaps, for people with dementia, we need more options for them.” She and her colleague said national strategies in other countries helped to raise awareness in sectors that were likely to come into contact with dementia sufferers, including shops, banks and bus drivers. Mr Forester-Morgan said: “You could build on what Bermuda already has, which is a strong community base, helping the community with understanding and how they can support somebody they know who is maybe displaying signs of dementia.” He added: “There’s so much community work that happens here, it would be great to have buddying systems for people who have been through the journey helping someone with dementia to remain involved in helping others.” Ms Stewart said the government teams had been “very supportive”. She added: “They know seniors are a huge issue for the island. It’s on their radar.” She admitted public funds were limited, but acknowledged that island organisations were making their own moves to come up with a plan. Ms Stewart said: “There’s a group of people who are going to start looking at creating a dementia strategy, which obviously we would pass on to the ministry.” A government spokeswoman said: “The ministry welcomes proposals for a dementia strategy aligned with WHO and PAHO priorities. The potential growth of this population is a key driver of prevention and addressing a long-term care system for the country.”
2018. November 20. The views of organisations that commented on proposed reforms to healthcare financing are expected to be made public in the next few weeks. Kim Wilson, the health minister, told MPs a task force set up to review two options first presented six years ago was to provide her with its views in the near future. The Minister of Health said it looked at the 2012 Report on a Health Financing Structure, which studied ways to improve healthcare financing and make it more efficient. In the earlier study, options were assessed based on a number of criteria, including their capacity to pool risk, financial strength, sustainability and ability to contain healthcare costs. At that time, it was thought that for a package of about $450 a month, an individual could be covered for local hospital treatment as well as some primary, long-term, overseas and dental care. Ms Wilson took the House of Assembly floor on Friday during a debate on the Throne Speech, which revealed her ministry wanted to develop a national health plan that will put everyone in Bermuda into either one or two health insurance pools. She explained that a “health financing reforms stakeholder consultation group” had been established that included Bermuda First, the Bermuda Chamber of Commerce, the Bermuda Hospitals Board, the Bermuda Diabetes Association, insurers, health professionals and international business. Ms Wilson explained: “Their mandate was to review the health financing options report and to provide the views of their stakeholder group on those two options. They also had the benefit of health economists to provide further overviews and further information if they so required it. I’m glad to say that the two-month process of their meetings has concluded, I’m expecting to receive a report from them probably within the next couple of days.” She said the group’s task was not to reach a joint position but to provide “different and rich viewpoints so that we could consider all of the options” and that MPs would hear more on the matter “in due course”. The Throne Speech also announced the Government would consult on the extension of paid maternity leave from eight weeks to 13. Ms Wilson said the consultation would allow the views of small businesses and others to be heard. However, Patricia Gordon-Pamplin, the shadow health minister, said an extension to maternity leave could be used by unscrupulous employers to target women. She explained: “We live in a misogynistic society and I would just hate for executives, HR people who are responsible for hiring to fulfil certain requirements in their company for employees, to decide that they start to discriminate ... you might find that HR person is saying, ‘I’m not going to hire that lady because in my estimation she’s of child-bearing age’, and they don’t want to run the risk of saying that perhaps we might find ourselves in a situation of having to provide maternity leave for this young woman.” Ms Gordon-Pamplin added it was important to consider the cost of healthcare provision alongside premium rates. The One Bermuda Alliance MP added: “We cannot effectively manage healthcare if we don’t look at both together.” Craig Cannonier, the Opposition leader, earlier proposed a public register to track the extent to which health services are used in a bid for “a more transparent and meaningful conversation” about which services are “over-utilized”.
2018. November 13. A Bill merging legislation for midwives with the Nursing Act 1997 has been tabled for legislation. If approved, the new Act would designate a joint council to regulate both, as well as a committee to field complaints for both professions. A code of conduct will be created for midwives, which had previously been governed under the Bermuda Medical Council. The Nursing Amendment Bill 2018 comes after the Ministry of Health acknowledged that midwifery on the island had been “limited due to an outdated regulatory framework”. The conjoined Nursing and Midwifery Council will have its corporate status removed, and the register will have a division for each category. Under the Act, only a registered midwife would be able to attend to a woman in childbirth, unless in cases of emergency or supervised by a registered medical practitioner.
2018. November 1. Black Bermudians with cancer symptoms are more at risk of death because they put off seeking medical advice, a leading British doctor has said. Jonathan Makanjuola, a specialist in urinary tract diseases, explained: “In my experience, people from African and Caribbean communities with possible symptoms of cancer tend to seek help late, potentially making the outcome much worse. “There are often cultural and religious reasons preventing black people from seeing their doctors early and this needs to change so that more lives can be saved.” Dr Makanjuola, a consultant urologist and lead clinician on bladder cancer at King’s College Hospital in London, was speaking as he prepared to visit Bermuda for consultation at the North Shore Medical & Aesthetics Centre in Devonshire next week. He said both men and women should “look before they flush” to check the colour of their urine as blood in urine is a key symptom of bladder and kidney cancer. Dr Makanjuola said that more than 10,000 people a year in England are given diagnoses of kidney cancer and about 8,000 people fall victim to bladder cancer. He added that more than 250 churches in England, including black majority churches and mosques, had backed a “Be Clear on Cancer” campaign designed to get people to check their urine colour. Dr Makanjuola said: “You should visit your doctor if you have blood in your urine, even if it’s just once.” He added: “The chances are it isn’t cancer, but it could be a sign of something else that needs treatment. If it is cancer, the sooner it is diagnosed the greater the chance of successful treatment. That’s why it’s important to pay attention to anything unusual happening to your body,” Dr Makanjuola is a consultant urologist and lead clinician for bladder cancer at King’s College Hospital in London. Dr Makanjuola was the first recipient of the British Association of Urological Surgeons/World Congress of Endourology fellowship. Dr Makanjuola is a member of the American Urology Association, the British Association of Orological Surgeons, and the European Association of Urology. He will be at the North Shore Medical & Aesthetics Centre from November 7 to 16.
• For more information, call 293-5476.
2018. October 22. Paramedics could save lives if they were introduced on the island, a Bermudian trained in the field in America has said. Gilbert Darrell, who was a paramedic in New York State, explained that the specialists have higher qualifications than emergency medical technicians and would be a valuable addition to the island’s emergency services because of the range of procedures they are trained to perform. He said: “Having paramedics can save an hour or two ahead of time. It has a really strong outcome for mortality and mobility. The emergency department can be maxed out as it only has a set number of doctors and nurses. If a patient comes in with a list of interventions already done such as IVs, fluids and medications, that really helps the physician.” Mr Darrell, who also worked as a firefighter and firefighting instructor in New York State and who has 18 years of experience in emergency services, said vital minutes could be saved if a paramedic was able to work on patients on the way to hospital. He added: “Load times into the ambulance can be five to 15 minutes even when you’re moving as fast as possible. Then add a 45-minute ride from the far ends of the island or even a five-minute ride from Hamilton and you have the ability to get life-saving care to the patient. You can give blood in the field. For a bad trauma, paramedics can give certain medications and blood products to keep a person’s blood pressure up and keep them alive before they get to the emergency room.” Mr Darrell said: “EMTs do a good job but they are missing two years of education and skills. An EMT has basic life-support skills like bleeding control, cardiac arrest procedures, CPR, logistics of the ambulance service — they are really first responders. Paramedics were designed to bring the ER to the field — to the patient. We have 50-plus drugs we can administer and a whole plethora of things that EMTs aren’t able to do because they aren’t trained.” He added that a paramedic qualification takes two years to complete and was a rewarding career. Mr Darrell said: “The great part about it is you get exposed to a tremendously high level of medicine without having to give up four years of your life in medical school and residency. There’s a certain amount of job satisfaction you get from providing acute care in the field and having a good level of autonomy. You are out there helping the community directly. A paramedic can make some life and death decisions by their own — it takes a certain caliber of person.” Mr Darrell, who now runs his own telecoms business, assisted at a serious crash in March, where he applied a tourniquet to a woman’s severe arm injury before she was taken to hospital. He is also a volunteer with charity St John Ambulance and provided emergency medical services for an America’s Cup team last year. Paramedics gained official recognition in Bermuda after a 2015 amendment to emergency services law, but there are none registered on the island at present. The Bermuda Hospitals Board said that it welcomed the use of paramedics — but that they were not vital in Bermuda because of its small size. A spokeswoman pointed to problems with keeping them certified due to the low number of patients that would need their help. She said: “Treating trauma patients in the ED is preferable to treating them on the scene. For this reason getting patients to the ED as quickly as possible is the model used in Bermuda.” She added: “In order to become a licensed or registered paramedic, individuals, in addition to course work, have to achieve a certain amount of practical experience. Keeping this experience current might be extremely difficult in Bermuda as the volume of serious trauma would not suffice for them to attain the required practical experience to retain their licence. Such individuals would be required to leave the island regularly just to clock practical hours and be considered safe to attend to patients locally.” The spokeswoman said: “BHB Emergency Medical Services and Fire Services have EMTs who function at a very high level. The emergency medical service is supervised by a medical director who is trained in managing all facets of acute unscheduled care.”
2018. October 19. Former health minister Jeanne Atherden has accused David Burt and Kim Wilson of lying to justify to taxpayers a $1.2 million public purse payout to Dr. Ewart Brown. The Opposition backbencher told The Royal Gazette that Mr Burt, the Premier and Minister of Finance, and health minister Kim Wilson were not telling the truth when they accused the former One Bermuda Alliance administration of ignoring the advice of the Bermuda Health Council over a reduction in fees for medical scans. “What is being said with respect to us having a vendetta and not listening to technical advice is not true,” Ms Atherden said. “It’s a lie and I put them to proof.” Former Progressive Labour Party premier Dr Brown owns two medical clinics which are set to receive more than $1.2 million from taxpayers as compensation for the fee cuts imposed by the OBA last year. The Bermuda Hospitals Board is expected to get $2.4 million for the same reason. Mr Burt and Ms Wilson have said the fee cuts were imposed to target Dr Brown, with the Premier describing them this month as an “economic vendetta” and the Minister of Health calling them “economic sanctions”. Mr Burt claimed the OBA Cabinet “disregarded the advice of the Bermuda Health Council”. Ms Wilson said the health council’s advice was to apply a new fairer methodology to the entire BHB fee structure and it was “extremely odd” that the OBA ignored that and applied it only to diagnostic imaging. Ms Atherden said neither had produced any evidence to show she ignored the advice she was given by technical officers at the health council, because the reverse was true. The health council, meanwhile, has refused to share with the public the advice it gave to her. “This business about a vendetta, I think that that is just so unbelievable,” she said. “The only thing I was targeting was the cost of healthcare.” She said it was hard to understand why public funds would be used to compensate private businesses whose owner chose voluntarily, as a provider of Standard Health Benefit services, to tie the fees he could charge to BHB’s fee schedule. “It is important that BHB only charges what it should charge and doesn’t get into the fact that other facilities are linked to its fees. The rationale for making these payments makes no sense to me. Where did that money come from?” Ms Atherden, a former Opposition leader, said when she was health minister she specifically asked the BHeC to look at whether the fees being charged at the King Edward VII Memorial Hospital for outpatient scans were appropriate. She was determined to bring them down because they had “gotten out of whack” over the years and were much higher than they needed to be. “The health council looked at it. They said they believed there should be some changes and if they implemented the changes, this is the impact in terms of the fee changes and the impact on the Standard Health Benefit. The health council are the ones that have the expertise in terms of looking at what type of charges should be paid, recognizing that they are able to make comparisons with other places, etc, in terms of what’s appropriate. I never got the schedule of fees. I never got into the nitty-gritty detail. Someone gave me a recommendation to say ‘put this in’ and I accepted it. I accepted the recommendation and said to Cabinet this is what was deemed appropriate at the time. You have got people talking about a vendetta but the bottom line is this: I was presented with an indication of how the fees would be changed ... and I accepted those proposed changes.” Ms Atherden said reducing the fees for scans meant health premiums did not go up for the “average man” — and that was the OBA’s focus. “If the fees being charged are wrong, you can’t say that just because somebody was getting too much that they have to keep getting too much,” she said. Dr Brown’s clinics, Bermuda Healthcare Services in Paget and the Brown-Darrell Clinic in Smith’s, are being investigated by police over allegations they ordered medically unnecessary tests for patients to boost profits. Dr Brown has denied the allegations. New fees for scans are due to come into effect on November 1. Neither Mr Burt nor Ms Wilson responded to a request for comment by press time.
2018. October 12. Bermuda Medical Specialties Group has added cosmetic plastic surgeon Peter Schwartz to its team of physicians. Board-certified by the American Board of Plastic Surgery, he specializes in cosmetic plastic surgery of the face, breast and body. Dr Schwartz is the chief of plastic surgery at Syosset Hospital. He also has privileges at North Shore University Hospital, Plainview Hospital and Glen Cove Hospital. With more than 20 years’ experience, Dr Schwartz specializes in various types of cosmetic plastic surgery procedures: facelifts, mini-facelifts, eyelid surgery, endoscopic surgery with small incisions, nose reshaping, breast augmentation/lift/reduction, liposuction, tummy tucks and many minimally invasive procedures. He also speaks fluent Italian, French and German. Dr Schwartz is a member of the American Society of Plastic and Reconstructive Surgeons, the American Society for Aesthetic Plastic Surgery, the Liposuction Society of North America, the New York State Medical Society and the Nassau County Medical Society. Arlene Basden, medical director at BMSG, which is based at 3 Reid Street, Hamilton, said: “In addition to improving one’s appearance, cosmetic plastic surgery can be a medical solution for matters such as back and shoulder pain, loose skin and disfigurement due to accidents.” Dr Basden added: “Residents of Bermuda demand access to a very high standard of medical care that many go overseas to receive it. We are very fortunate that Dr Schwartz has made his talent available to us in Bermuda.” Dr Schwartz said: “The highest concern in my practice is the exceptional and individualized care of our patients, before, during and after cosmetic plastic surgery to improve their self-image and boost their self-esteem. Personalized excellence in cosmetic plastic surgery procedures is delivered through a continuous quest for outstanding medical knowledge with continuing education, combined with an artistic sense and use of the latest proven technological advances in cosmetic plastic surgery.”
2018. October 4. The Bermuda Health Council has refused to reveal the advice it gave former health minister Jeanne Atherden before the One Bermuda Alliance government decided to slash fees for scans last year. Tawanna Wedderburn, the health council’s chief executive officer, said: “The health council has no comment on the matter at this time.” Mrs Wedderburn was speaking after David Burt, the Premier, and Kim Wilson, the Minister of Health, claimed the health council’s recommendation on how much healthcare providers should charge for CT and MRI scans was ignored by Ms Atherden before last year’s election. They alleged she instead imposed bigger cuts in June 2017, which caused a sharp drop in income for the Bermuda Hospitals Board and Ewart Brown, a doctor and a former Progressive Labour Party premier. But Ms Atherden insisted the claims were a “false accusation” and questioned why the PLP, when in Opposition, did not object to the change in fees for scans when a Bill was passed in Parliament last May. The Government has said it expects to pay out a total of $3.6 million in compensation for lost revenue because of the fee cuts — $2.4 million to BHB and $1.2 million to Dr Brown. The Royal Gazette asked the health council last month to reveal the advice it gave the minister and if it differed from the fees that were set. Ms Wedderburn said at the time: “As public officers and per the Bermuda Health Council Act, the secretariat does provide advice to the Ministry of Health.” She added: “In a recent survey by the health council, the public asked us to be more transparent. As a result, our internal policy about information release is under review to increase transparency and the public’s understanding about our role, including in determining reimbursement rates. We will provide any information we can in due course. Our policy to release information is being reviewed, including information about technical advice.” New Opposition leader Craig Cannonier stepped into the row over compensation for the fee cuts at the weekend. He said the payments to “wealthy” Dr Brown were “Robin Hood in reverse”. But Mr Burt said: “Given the Opposition leader seems to now like the truth, he should start by telling the truth about why this vendetta was approved by him in Cabinet. The Opposition leader should explain to the people of Bermuda how he sat in a Cabinet that disregarded the advice of the Bermuda Health Council and approved this economic vendetta which negatively affected the hospital and caused this $3.6 million liability for the taxpayers of Bermuda.” The document listed the fees set by the OBA on June 1 last year and a list of higher recommended fees — with the difference in price shown for each procedure. The difference was only $90 in some cases and in others more than $450. The difference is what the Government is paying to Dr Brown and the BHB for each procedure they carry out until new higher fees come into effect on November 1. Neither the ministry nor the health council responded to questions yesterday on whether the list of higher recommended fees shown in the analysis formed part of the advice the BHeC gave to the former minister. Ms Atherden also failed to respond to a request for comment.
2018. October 1. A healthcare worker is under investigation for allegations of inappropriate sexual behavior involving a child, the Bermuda Health Council has announced. A statement follows: "The Bermuda Health Council recently received information about an unregulated health professional who allegedly engaged in inappropriate touching of a sexual nature with a child. The allegations are being investigated as the council referred the matter to relevant authorities. In light of this allegation, the health council reminds the public to check if your health professional is registered, and practices in a safe facility before you receive healthcare." Tawanna Wedderburn, CEO states: “The health council supports safe, quality care. Through a recent survey we conducted, the public asked us to speak up. We are meeting that request. Unusually, we are taking this step to highlight this information because of the risks faced by the public including children and other young people. Generally, no one has the authority to check most health facilities or the practices of unregulated health professionals. It is important that there is adequate oversight of those delivering health services. We view this serious information not only as important information to share but as an opportunity to improve our health system and protect the public from future harm. We are partnering with agencies in the community to do research and will keep advocating for what is best for the health of Bermuda. The health council may be limited by our legislation to act on these matters, but we support the public in asking questions about their care and will always listen. We are also liaising with professional associations to encourage greater oversight of unregulated professionals. We encourage the public to contact us anytime they are concerned. Regulated health professionals include physicians, nurses, pharmacists, dentists, allied health professionals, optometrists/opticians, and midwives. Unregulated professionals include those who practice acupuncture, massage therapy, chiropractic, social work, counselling, naturopathy, and various assistants to regulated health professionals (e.g. physiotherapy assistant). If you need to know which health professionals are registered to deliver care in Bermuda, visit our website or call 292-6420. The health council will continue, as always, to advocate for the changes Bermuda’s health system requires."
2018. September 26. The waiting list for CT scans has not increased since one of the island’s two scanners was shut down, the Bermuda Hospitals Board has said. Ewart Brown, a doctor and former premier, said this week he was to reopen the CT unit at his Brown-Darrell Clinic in Smith’s after a nine-month closure because of “public demand for quicker access to exams and reports”. But the BHB earlier told The Royal Gazette there had been no change in waiting times for patients in need of a diagnostic CT scan since Dr Brown’s unit closed in January. Figures provided by the board showed only a small increase in the number of CT scans carried out at the King Edward VII Memorial Hospital in the six-month period after the closure of the Brown-Darrell unit, compared with the same period in 2017. There were 6,808 CT scans carried out between February and July 2018, compared with 6,775 between February and July last year. A BHB spokeswoman said: “Although numbers have gone up slightly, there has been no change in wait times for this time period. Currently, it is just under two weeks for elective, that is planned, CT scans. Emergency referrals are not subject to a wait time and are undertaken as needed.” Dr Brown said his decision to reopen the unit was also based on the Government’s plan to increase fees for scans after they were slashed by the former One Bermuda Alliance administration last year. He claimed there was a backlog of about two weeks for patients to get CT scans at the hospital while his equipment was shut down. Dr Brown said: “That’s not unusual for hospital based CT scans. They never know how much traffic they’re going to have from the emergency room or from inpatients. Those are always higher priority than outpatients. It shows that the island needs another CT.” Dr Brown added he had received calls and e-mails about the delays on “a daily basis”. He said: “My information is that the wait at the hospital is two weeks. When we open, with both places working efficiently, Bermudians can have their scans done within days, not weeks.” Tawanna Wedderburn, chief executive of the Bermuda Health Council, told The Royal Gazette last week: “There is no guideline on how many CT scanners per population a country should have, although the World Health Organisation and the Organisation for Economic Co-operation and Development track data for each country. If there are not enough CT scanners in Bermuda, there will be wait times, people may get sicker, and people will not have choice in where to receive care. If there are too many CT scanners, people may be exposed to too much unnecessary testing and healthcare costs will increase.” She added: “Bermuda has three scanners — two at BHB and one at the Brown-Darrell clinic. There are two scanners in use today and that is the two at the hospital. The availability of CT scanners is higher in Bermuda than other countries, when two scanners are available for use. Current capacity in the health system can meet the demand of an ageing population, enabling people to receive care without compromising quality.” Dr Brown closed the unit at Brown-Darrell at the end of January. The closure followed a government grant of $120,000 to the Brown-Darrell Clinic and another of $480,000 to Dr Brown’s other clinic, Bermuda Healthcare Services in Paget, which has an MRI machine. The new increased scan fees will come into force on November 1 and Dr Brown announced on Monday that CT scanning would resume at Brown-Darrell two days later. He said that up until June 2017, Brown-Darrell was a “busy” clinic. But he said the fee reductions meant the practice took a huge financial hit, with procedures charged at far lower rates — more than 80 per cent less in some cases. Bermuda Health Council has insisted the fees were cut as part of a bid to drive down healthcare costs. Dr Brown claimed the impact of diagnostic imaging on healthcare costs was “blown vastly out of proportion”. He repeated allegations that the health council recommended the cuts as part of a “political vendetta” against him. The health council has denied the claim. JJ Soares, a GP who joined Dr Brown last October to threaten legal action against the Government over the fee cuts, is scheduled to open a clinic in Hamilton to offer MRI and CT scans. Ms Wedderburn said the two MRI machines already in use at KEMH and Bermuda Healthcare Services were enough to “meet demand without compromising quality”.
2018. September 25. Bermuda Hospitals Board (BHB) Nurse Practitioner Myrian Balitian-Dill is one of only a handful of registered nurses who have attained nurse practitioner designation in Bermuda. She is now the first to be granted authority to write prescriptions locally. Mrs Balitian-Dill received the news from the Bermuda Pharmacy Council on 31 August 2018. Mrs Balitian-Dill is the only nurse practitioner at BHB. On obtaining her qualification she moved into a nurse practitioner role in the hospital’s Cardiology Department. In November 2016 she transitioned to help set up a new service at BHB, the Patient-Centred Medical Home. The small dynamic team of this service also includes a physician medical director, a staff nurse and an office administrator. The setting provided the ideal environment for Mrs Balitian-Dill to be afforded the right to prescribe as Bermuda legislation dictates that prescribing rights can be granted to nurse practitioners “under the authority of a medical practitioner”. The new development is the result of several years of collaboration to ensure all the necessary regulatory documents were in place. Mrs Balitian-Dill is pleased with the move and sees it as a starting point and an important way to help reduce health care costs. While the permission only exists under the direct supervision of a physician, Mrs Balitian-Dill explains the benefit. “I believe it makes the system more efficient. If the nurse practitioner can prescribe evidence-based therapy at point of care, why do we need to wait for another practitioner (physician) to prescribe that therapy?” I applaud the path Myrian has taken in her nursing career,” said BHB Chief of Nursing Judy Richardson. “Myrian is passionate about advancing nursing practice in Bermuda. Her work with the Patient Centered Medical Home is yielding positive results. Early evidence shows improved health of clinic patients who had frequently used other services. Our Clinical Services Plan identified the need for a more diverse workforce which includes more advanced practice nurses like Mrs. Balitian-Dill.” BHB CEO Venetta Symonds said: “We welcome this move by the Pharmacy Council and are proud of Myrian’s accomplishments and her dedication to provide our patients with the best possible care.”
2018. September 20. A new approach to healthcare that could save money and prevent more people becoming sick is to be presented tonight at a dinner for doctors. Henry Dowling, who said he could be the island’s only physician to adopt the direct primary care model, billed his talk as offering “a solution to our healthcare dilemmas”. He said: “We want to go back to taking care of the whole patient, and not waiting for people to get sick, or referring them to somebody else because we can’t take the time they need. I didn’t go into medicine to mop up problems. I want to fix the problems.” Dr Dowling is to speak on direct primary care at the Bermuda Healthcare Services and Brown-Darrell Clinic’s quarterly Docs for Dinner event. The Paget-based doctor said that direct primary care involved payment of a flat monthly rate to cover visits to the practice. He explained: “Direct primary care is considered membership-based care. Patients play a flat fee per month, and get unlimited visits per month and access to their doctor.” Dr Dowling added: “It’s grown in popularity in the States, where there are around 800 practitioners involved. Five years ago there were maybe half that. It was borne out of the frustration of primary care doctors that were ending up with more paperwork and seeing more patients just to keep their doors open.” Dr Dowling said the island’s model was a fee for service system based on patients “coming to us with a problem”. He added he started to explore direct primary care after he became “frustrated with everyone talking about the cost of healthcare, but with no meaningful change”. The Bermuda Health Council’s annual reports have tracked the ever-rising expense of healthcare. The BHeC earlier this year tallied healthcare spending at more than $700 million from April 1, 2015 to March 31, 2016. The watchdog warned at the time that the island’s healthcare system was “at a breaking point”. Dr Dowling, who returned to the island in 2002 after working at a family practice in New Jersey, said he had grown disenchanted with the business of medicine in Bermuda. He said: “I started looking for alternatives. Direct primary care meant, more or less, going back to the old family doctor who did everything for the family. It goes back to what I trained for. Patients don’t just go to the doctor because they’re sick, but to stay healthy.” A general physician at Associates in Integrated Health and Bermuda Chiropractic Health Centre, Dr Dowling said he had switched to the new model in May. He added: “A patient’s fee is anything from $20 a month to the most expensive of $105. It’s not going to cover things that happen at the hospital, lab work or X-rays. It covers you seeing the doctor, seldom for less than half an hour or 45 minutes. I guarantee same-day access and access to me after hours. That potentially can offset some of these emergency room visits.” He added the most “basic” visit to the emergency room at the hospital costs “$450, minimum”. Dr Dowling said: “Direct primary care has been shown to save money to the healthcare system. It’s not about making money but about establishing relationships.” He added the move also cut out dealing with insurance companies. He said: “I leave that for patients to use elsewhere. I have approached some insurance companies and they are not with the idea, which is surprising. In the States, there are some insurers that will reimburse patients monthly because it benefits them if patients are not having to access high-cost healthcare.” The talk, open to invited guests only, will be held from 7pm at the St George Room at Café Lido at Elbow Beach.
2018. September 19. A doctor who joined forces with former premier Ewart Brown to threaten legal action against the Government over a cut in medical scan fees is to open a new clinic to provide MRI and CT imaging. JJ Soares warned last year that plans for the walk-in centre on Burnaby Street might have to be scrapped because of the fee reductions imposed by the former One Bermuda Alliance administration. However, he told The Royal Gazette in an e-mail that a pledge by the Government to increase the fees meant the project would go ahead. Dr Soares said: “Our plans to open the walk-in/urgent care centre on Burnaby Street in Hamilton are moving forward and nearing completion. “It will operate seven days a week, open from 6.45am to 10pm, and will offer access to all diagnostics, including MRI, CT, ultrasound, X-ray, mammography and cardiac diagnostics, as well as blood testing.” He added: “It is our understanding that the previous drastic and unsustainable cuts to reimbursement for MRI and CT scans are in the process of being revised upwards by the current government.” Dr Soares sent a letter to the Government threatening legal action regarding the fee cuts last October, along with Dr Brown. Their complaint was that the reductions, recommended by the Bermuda Health Council to reduce healthcare costs, would hit their businesses. A lawsuit was avoided after the Cabinet approved compensation of $600,000 for Dr Brown’s two medical practices, Bermuda Healthcare Services in Paget and the Brown-Darrell Clinic in Smith’s. The Ministry of Health said the “financial supplements” paid to Dr Brown’s clinics, and a supplement of $1.8 million to the Bermuda Hospitals Board, were granted “in order to help ensure CT and MRI services are readily available to the public”. The ministry made the statement the same day Dr Brown announced he would close the CT scan unit at the Brown-Darrell clinic at the end of January this year. A disclosure by the Ministry of Health under public access to information revealed that Dr Soares, unlike Dr Brown, did not receive compensation from the public purse. The Pati release included an e-mail from Jennifer Attride-Stirling, the health permanent secretary, to Kim Wilson, the Minister of Health, on January 23 this year, which contained draft responses to media questions. Dr Attride-Stirling wrote: “The ministry can confirm that a letter before action was received in relation to the fee levels. However, as the matter was settled via legal counsel, details about the particulars of the action will not be provided. One other practice joined Dr Brown in the letter before action. There was no grounds to that claim.” Dr Soares declined to comment on his claim and referred questions to his lawyer, Jerome Lynch QC, who said: “Dr Soares does not yet have an MRI or CT scanning service, so no claim for losses as yet arise from a cut in fees, although the Bermuda Health Council are well aware of the doctor’s plans. He is understandably concerned about the appearance of arbitrary action by them that may affect those plans and will do whatever is necessary to ensure the people of Bermuda are not denied the best value medical service for political reasons. The Government are once again considering a fair fee structure which we anticipated being published on October 1. We remain optimistic that good sense will prevail.” An earlier Pati disclosure showed that Dr Soares met with Ms Wilson on September 13 last year to discuss the new urgent care centre. A record held by the Ministry of Health about the meeting said he asked the minister to “support the project as it will provide an extension of needed service after hours and during weekends. But the UCC will only work if he has the full range of diagnostic services. He asks if the minister can’t endorse it to at least not put anything in place that will thwart it.” The note added: “The minister thanked him for the presentation, noting the issue with MRI and CT fees remains a pending issue.” Dr Soares also told Ms Wilson the fees for MRIs were not high enough. The note said he “estimated the cost impact of his MRI, the electricity bill alone will be $17,000 per month, so a $450 fee for a brain MRI is just not enough. There are staggering costs associated with it.” Dr Soares told The Royal Gazette his new clinic would offer Bermuda’s only “truly open” MRI unit. He said it would help claustrophobic and obese patients and would reduce patient wait times for an MRI or CT scan. Dr Soares added: “We will offer appointments for MRI, CT and other diagnostics on a ‘walk-in’ basis when possible and certainly within a few days of request. Currently, the wait time for an MRI or CT at the hospital is anywhere from two to four weeks. We believe that the Bermuda public deserves better and we plan to deliver.” The GP added: “Urgent care patients will be able to walk in and be seen without any appointment for a mere fraction of what it costs to be seen at the emergency department, thereby saving healthcare dollars.” A BHB spokeswoman said the present wait time was less than two weeks for planned, elective CT scans at King Edward VII Memorial Hospital. She added: “Emergency referrals are not subject to a wait time and are undertaken as needed.”
2018. September 6. In June 2018, the Bermuda Health Council conducted a survey to capture the public’s opinion about healthcare issues and the Health Council’s role in tackling these issues. Over 550 people responded, representing varied education levels, professional backgrounds, races and genders, but with one resounding unified message - Healthcare in Bermuda is too expensive and it needs to be at the top of the Council’s list to do something about it. Over 75% of respondents felt the role of the Health Council is to protect the public by making healthcare affordable, particularly with health insurance premiums, cost of care and the price of medications; and to monitor and report on Bermuda’s healthcare state of affairs. Respondents felt that the Health Council is a source for useful information and evidence based policy, with “valuable insight” (53%). However, it was noted that the information could be communicated more effectively with improvements in the frequency and availability of information to the public and healthcare providers (both were prioritized by over 68% of respondents). Respondents also felt that there are opportunities for stronger regulation of healthcare. Overall, the Council needs to do more in these areas to make it clear what their role is and how they act on behalf of Bermuda. As one concerned respondent stated, “I have heard of the Health Council, but that’s it.” The Council is committed to ensuring transparency and reliability of messages and that appropriate actions are taken towards improving the affordability of healthcare. In support of the feedback, the Council recently held a strategic planning session which saw the team prioritizing its work on health legislation to ensure care can be delivered in more cost effective community settings, and expediting regulations to control the price of prescription medicines. Tara Hines, Healthcare Data Analyst stated: “The results we received from the 2018 Bermuda Health Council Feedback Survey confirm much of what we are seeing on a daily basis in our research, with regard to healthcare costs. In order to make sure more people know about the work that we are doing and that they can access information they may need, we have created a Data Request Form on our website (www.bhec.bm) and we provide regular updates online about what our team is working on in our Behind the Scenes Activity Log. We are also using data, in collaboration with the broader healthcare community, to find ways to provide more public value for the dollars being spent.”
2018. July 30. A 6.4 per cent increase in the standard premium health insurance rate was caused by an increased need for healthcare rather than an increase in fees, the health minister said. Kim Wilson told the House of Assembly that Government will continue to work to address the root causes of the hike. Ms Wilson said: “We have been accused of reneging on our promise to contain healthcare costs but I think all informed parties understand very well that the 6.4 per cent rise in the standard premium was due to increased use of services in the previous year. That is utilization that could not have been prevented by this government.” She added: “Going forward, we have demonstrated our commitment to containing health costs by not increasing standard benefit fees, in particular for the largest provider, the hospital. And, rather, we have undertaken the difficult work to modernize BHB’s fees to be based on an international standard of relative value units with a local conversion factor.” Ms Wilson said the work was in its final stages and would be brought to the House later this year. She also gave MPs an update on the ministry’s work over the past year to improve the standards of care homes and daycare facilities through legislation. She said her ministry had introduced sugar tax legislation after consultation. Ms Wilson said: “The legislation allows for local producers of food to be exempted from the tax. This means local vendors like bakers, snowball stands and so on, won’t be impacted. In fact, local food producers are better off because the new concession can be used to purchase their equipment as well, not just the sugar. However, the initiative contributes to the Government’s commitment to incentivise the public to choose healthier options in order to battle Bermuda’s overweight and obesity problem.” Ms Wilson added the Government had established an obesity and diabetes scheme to tackle habits that lead to chronic diseases. She thanked the previous OBA administration for their efforts to deal with the island’s health problems. Ms Wilson said: “I want to acknowledge the good work of the previous administration, which established some great initiatives that we are happy to continue, such as the review of the mental health act and the long-term care action plan. They also advanced many initiatives that were started under the previous PLP government, such as FutureCare and the Bermuda Health Strategy, which have become central parts of our health system. This shows that bipartisan agreement and collaboration serves to achieve the country’s best interest and is an effective way to bring about long-term improvements in health and healthcare for Bermuda.” Ms Wilson urged the public to be safe and responsible over the Cup Match holiday. She said: “Without wanting to rain on the parade, I do have to pause and remind us all that drunk driving and sexual indiscretions increase dramatically during any public holiday. We relax, overindulge and take risks — risks that can cost us our life. Accidents go up during any public holiday, and visits to the Communicable Disease Clinic go up immediately after such holidays. So let us take heed of past experience and celebrate this Emancipation Day by freeing ourselves of thoughtless decisions that hurt us and our families.”
2018. July 25. A new addition to Bermuda Hospitals Board’s cancer care staff will bring decades of experience to Bermuda. Christopher Price was named as the new consultant medical oncologist by BHB this afternoon. The addition of Dr Price brings the number of full time oncologists on staff to three. Michael Richmond, chief of staff at BHB, said that the organisation was “delighted” to welcome Dr Price. Dr Richmond added: “The addition of Dr Price to the team is evidence of our commitment to provide treatment locally for our cancer patients. We recognize the ability to be at home and close to family and friends is an important aspect of cancer care and it is one that Dr Price has much experience in.” Dr Price said he had been impressed by both Bermuda’s beauty as well as the “obvious pride of staff in the excellent local health services” during a visit last November. He added: “The ambition of BHB and the KEMH Oncology Department to offer high-quality cancer care to local residents on the island wherever possible, in partnership with local charities and where appropriate with external institutions in North America, was very clear. “I was delighted to be given the opportunity to contribute.” Dr Price served as director of research and development at Worcestershire Acute Hospitals from 2014 to 2018 and clinical service lead for oncology from 2017 to 2018. He worked the Worcestershire Royal Hospital to help develop a new oncology department in 2014. He served as director of medical oncology training to the UK’s South West region from 2003 to 2013. Dr Price was appointed consultant medical oncologist at University Hospitals Bristol in 1995.
2018. July 23. Almost half the Bermuda’s population has one or two chronic disease challenges, and that is a major factor in the $701 million annual cost of healthcare on the island. Data shows that 45 per cent of the island’s residents fall into that category, and 20 per cent of the population with a chronic disease consume 80 per cent of island’s healthcare dollars, according to Alison Hill, chief executive officer of Argus Group Holdings. As one of Bermuda’s major providers of health insurance, the company is at the forefront of efforts to address the rising cost of healthcare — a problem that is being faced around the world. Argus is taking a two-pronged approach that is partially focused on supporting people to look after their health, and partially on finding ways to reduce healthcare costs. Kim Wilson, Minister of Health, highlighted rising health insurance premiums — up as much as 18.5 per cent — when she spoke about the impact of the soaring costs in the House of Assembly on July 6. The Bermuda Government is working on health reform proposals, including a draft benefit package. Ms Wilson blamed the rising costs in part on the population being sicker, older and receiving more healthcare. Against that backdrop, Ms Hill has described efforts by Argus Group to address the challenges. She said healthcare inflation globally is about 8.4 per cent, “about three times the level of inflation. It is just not sustainable”. Healthcare costs in the US are projected to increase 6.5 per cent this year, while the standard health benefits in Bermuda have increased by 6.4 per cent. For comparison, Bermuda’s inflation rate was 1.9 per cent last year. Ms Hill explained that of the $701 million the island spends on healthcare, 12 per cent goes to overseas health providers, 46 per cent goes to the King Edward VII Memorial Hospital and the rest to local healthcare providers and administration. “So there is a lot that we can do in Bermuda to bring that cost of healthcare to a more sustainable level,” said Ms Hill. One of the things Argus is doing is working in partnership with local providers to create “a fee for health outcomes model” rather than a fee for service model. Ms Hill said Argus was proud of the diabetes-reversal programme it is doing in partnership with Hamilton-based Premier Health. “We are delivering real, tangible benefits. It is in its early stages, but for the cohort that has gone through we are seeing on average $1,000 per head saving on prescription drugs and we have seen an average weight loss reduction in that group of about 12.7lbs,” she said. Another example of how the insurance company is advocating for health is its nurse case management programme, which assists insured clients with multiple chronic conditions to better manage their health. Ms Hill said that as people go through the programme the company has seen annual healthcare reductions of more than $6,500 per individual. “So we know if we use technology and that personal touch and work with our insureds and encourage them to really adopt positive changes to their health, the economics of it work — and we offer all of this stuff essentially for free. We know that a short-term cost will generate a long-term benefit,” said Ms Hill. A healthier population and a reduction in the cost of healthcare will also have wider benefits for the island, as it would make Bermuda a more attractive place for job creation and foreign investment, according to Ms Hill. She said: “Attracting healthy people to the island really helps address that demographic change of an ageing population and chronic disease. Health insurance is a huge part of the cost of employing someone. Making those health dollars work as efficiently and as cost effectively as possible is what we are constantly striving to do.” Peter Dunkerley, chief financial officer, said: “For the company we are very optimistic for the future. The position we are in now, having taken some of the actions we have taken, is good for a very long time.” He was referring to, in part, a restructuring of the company’s balance sheet, which included moving out of a number of noncore, illiquid assets. This involved write-downs of $19.5 million. On Friday, Argus reported a net loss of $18.6 million for the year end. Mr Dunkerley said taking a short-term loss would “generate the best long-term value for our shareholders and all our stakeholders”. He also said: “We can also really focus on dealing with some of these key issues that Alison has highlighted — creating seamless, cost-efficient back-office infrastructure, and working more with our clients to improve their physical health and financial health.” Beyond health insurance, Argus Group also offers a number of other services, including property and casualty insurance, pensions and investments, and wealth management.
2018. July 21. Bermuda could become a centre for specialist colon removal surgery, a surgeon at the Bermuda Hospitals Board has said. Fitzroy Hamilton said results in Bermuda were better than those of top European clinics that use single-incision laparoscopic surgery for colon removal. Dr Hamilton said: “What we have seen from reviewing 186 cases we have done is that we have the outcome to show that we are very much on par with the guys in Europe and even better.” He added: “We are leading in our outcome and I think we should explore making Bermuda the destination for patients for Sils colon surgery not only for medical tourism, but also the possibility to train surgeons in the diaspora. We should try to make Bermuda a centre of excellence for Sils colon surgery.” Dr Hamilton said Bermuda is already a leading centre for the procedure on this side of the world. Dr Hamilton explained that the procedure involves the use of a single point to get into the abdomen and remove the diseased part of the large intestine. He said the method shortens the amount of time patients have to spend in hospital and “significantly” reduces the risk of complications. Dr Hamilton said: “It is widely expected that you are going to have complication rates roughly up to 13 to 14 per cent in any population that does this procedure. He added: “Our complication rate was 11 per cent.” Dr Hamilton said operating times were also faster, at an average of about 130 minutes, “which is the bottom of normal”. He added: “Everyone knows the procedure now, so it flows, so your operating time is less, the patient stays on the table less, there is less anesthesia, less operating time, less risk.” Dr Hamilton explained that male patients and those who are overweight or obese are at greater risk of complications. “In Bermuda, we are dealing with two out of three people with a body mass index over 25 so we have a third obese, a third overweight. So off the bat, we are expecting worse outcomes. Not so based on our findings.” He explained that patients can be rejected for the surgery in other parts of the world if they are too sick or overweight. “We don’t have that luxury. We are in the middle of the Atlantic. There is no second or third-choice hospital.” For the patients, who for the most part we think are fit enough for surgery, we do the procedure with excellent outcomes.” Dr Hamilton said the results showed that this surgery “can be done in patients who are sick, who are advanced in age, who are a little heavier than normal, with great outcomes”. He put Bermuda’s success down to skilled surgeons performing the procedure on-island and experienced operating-room staff. Dr Hamilton added: “Safety comes first. We have a safe procedure, great outcomes and very capable surgeons so nobody needs to go overseas for colon surgery.” He said Sils surgery, widely used in Europe but less so in the United States, had become the mainstay for colon removal in Bermuda since it was introduced on a large scale in 2012. “Dr Boris Vestweber, who is world renowned in this procedure, was integral in getting the procedure accepted here. Now there are five surgeons in the hospital and they all do the procedure in varying degrees. Four of them learnt the procedure here on-island.” Dr Hamilton said the team are now looking to publish their results. He added: “This procedure has never been studied in any population this size, in such a remote setting with such a small population. But this population is rich for this procedure because of the diseases we find, because of the age of the patients, because of the size of the patients. The main focus of this and what we want everybody to see is that this can be done anywhere once you have surgeons who can be trained in the use of the port.”
2018. July 7. Health insurance premiums have spiked as much as 18.5 per cent, health minister Kim Wilson told MPs yesterday. In some cases this will mean residents having to pay an additional $100 a month, which Ms Wilson said “can’t be easy for most working families”. She cautioned: “We are not here to blame insurance companies or the previous government.” Ms Wilson blamed the rise in part on the population being “sicker, older and receiving more healthcare”. The island’s most basic package, the standard health benefit, covers only hospital and “a few non-hospital services”, MPs heard. The rest, she said, was priced in “tiny pools among small and medium-sized employers, or individuals without group coverage — they are the most exposed of all”. Bipartisan health reform proposals to stabilize health costs have left the Government with two options for advancement, as well as a draft benefit package now under review. That draft package, dating back to 2012, envisaged a “solid, decent” health plan requiring around $450 a month per person. Although prices had risen in the five years since, Ms Wilson said changes to the “basic package and pool” of health insurance would avert small groups taking sudden steep premium rises. She added: “That is what my technical teams are working on, and I will be pleased to come back to my honourable colleagues and update you again in the coming months.” Ms Wilson noted smaller reforms achieved over the last three years, such as the “dramatic” reduction in fees for long-term hospital care. In particular, the enhanced care pilot programme targeting chronic disease such as diabetes, in place since February 2017. had seen 206 patients enrolled to date. Participants had “substantial” reductions in emergency department and hospital admissions, Ms Wilson said, praising the “bipartisan genesis” of the scheme.
2018. July 6. The island’s general hospital, King Edward VII Memorial, logged 430 incidents that resulted in harm to patients over less than five years, Bermuda Hospitals Board statistics have revealed. Of those, 28 fell into the three most serious categories of harm — 14 patients died unexpectedly, 5 needed life-saving treatment and 9 suffered permanent harm as a result. The figures were included in statistics released by BHB that showed there were 4,090 incidents reported by staff at the King Edward VII Memorial Hospital between March 28, 2011 and December 31, 2015. The number of reported incidents that involved patients is far higher than earlier reported by the hospitals board. The most common events involved falls or slips and medication errors. BHB released data in December 2015, in response to a public access to information request from The Royal Gazette, which logged only 13 events between 2011 and 2015. Michael Richmond, BHB’s chief of staff, said yesterday that the number of reported adverse events at the hospital was comparable with similar institutions overseas, based on his experience, although there was no established international benchmark. He added that any adverse events had to be viewed as potential for improvement and were taken seriously. Dr Richmond said it was unwise to over-interpret the data, because it only included incidents that staff reported. He explained that some incidents would not be reported and that many credible articles suggested only 15 percent of events were picked up by hospital reporting systems. He said: “Reporting systems are notoriously weak and inconsistent in identifying all harm events.” A total of 534 incidents were reported at KEMH amid about 6,000 hospital admissions, 30,000 emergency department attendances and 6,300 outpatient procedures last year. There were 900 reported events in 2012, against a backdrop of similar hospital activity. The World Health Organisation says European data consistently shows that medical errors and healthcare-related adverse events occur in 8 to 12 per cent of hospitalizations. Dr Richmond said he was unable to provide the numbers to enable a comparable rate to be calculated for KEMH but it may be possible in the future. He said he was less concerned about how the figures compared internationally and more worried that the number of reported events at KEMH was falling because of a failure to report. He said: “I’m very worried that we have got a reduced level of reports.” He added that his aim was to create a culture at the hospital where reporting was encouraged because that would lead to improvements in patient safety. “We are putting a system in place where the frontline staff are the eyes and ears of the organisation.” He added that specific projects had been launched to target the most common kinds of accidents and errors. The chief of staff said the figures released to The Royal Gazette in 2015 included only those incidents in the “sentinel events” category — those that could have or did lead to unnecessary death or major harm and could have been prevented. “There was no effort to mislead. That was the way it [the Pati request] was interpreted by whoever. It would appear that the numbers were low.” He said the 13 sentinel events were a subset of the 4,090 reported adverse events. Dr Richmond added that the board did not have data showing how many of the remaining 4,077 events were preventable or had involved hospital error —although each logged incident was reviewed to determine what happened and action was taken if needed. Dr Richmond, who joined BHB last July, said “many” of the incidents probably were preventable and the board was working towards a system where it was possible to identify the exact number. He admitted the sentinel events category was “probably ... too narrow” to provide the public and the board with the information it needed about avoidable incidents. Dr Richmond said: “We clearly have events that are happening that are preventable. We are an organisation that has a clear ambition to be the safest hospital we possibly can. The way to do that is to interrogate your data, to share your data and to learn from your data. Are we an exemplary organisation? I am saying 100 per cent not. We are an organisation that has to reduce harm. That is in our quality improvement strategy. We have a system that is maturing and improving. I would like for our systems to be able to give us that data.” Dr Richmond, who is responsible for quality of care at the hospital, pledged that BHB would publish its incident statistics twice-yearly on its website in the future. He said: “Our aim is to be fully transparent. Really, as a consequence of you pushing and trying to get the information, we have said ‘why aren’t we putting our data on the website to allow the public to be informed?’ And we will. This is information we must be held accountable for and the public have a right to know it.” As well as the information on reported adverse events for 2011 to 2015, BHB’s new figures provided more up-to-date statistics. They show that between March 28, 2011 and May 31 this year, 5,483 adverse events were reported at KEMH, with the majority — 3,644 — involving no harm. There were 663 events that did involve harm, with 41 incidents that fell into the three most serious categories of harm. A total of 18 patients died unexpectedly, 8 patients needed life-saving treatment and 15 suffered permanent harm over the period. There were 1,167 incidents where the severity level was unknown or not identified — it is not mandatory to assign a severity level. There were also nine deaths which were “not caused by a safety event”. Dr Richmond said after the incident log was reviewed, it was probable that the severity levels would have changed in only between 5 and 10 per cent of cases. The Royal Gazette first asked BHB for statistics on “serious untoward incidents” at KEMH in the previous five years in September 2015. The request listed terms which the events could have been recorded as — phrases used in healthcare to describe incidents involving avoidable harm, including “sentinel” and “adverse”. The request was aimed at ensuring the broadest possible range of incidents was disclosed. After BHB released information on only 13 events, The Royal Gazette asked for an internal review by Peter Everson, then the BHB chairman. Mr Everson upheld the board’s decision, but The Royal Gazette appealed to the Information Commissioner’s Office. The latest disclosure followed a request from the ICO to BHB as part of a negotiated resolution.
2018. June 29. The standard premium for health insurance is to increase because demand for medical treatment has continued to rise. Kim Wilson, the Minister of Health, said the standard premium rate, mandated for all insurance packages, would go up by $21.31 to $355.31 per month. The increase is in contrast to the $4 decrease put in place last year. Ms Wilson said: “Increasing premiums is not something any Government does lightly. “However, we have seen significant increases in the use of services caused by the high incidence of chronic, non-communicable diseases and the ageing of our population. The sicker our people are, the more it costs to care for us, and the higher premiums become. It is a simple and preventable cycle we have to get out of.” She was speaking as the House of Assembly debated the Health Insurance Amendment Act (No 2) 2018 last Friday. The minister said the Bill included changes to the Mutual Reinsurance Fund and its coverage for kidney health. The Bill will increase the coverage of kidney transplants from $100,000 to $150,000 to help more people get surgery. Ms Wilson said Bermuda Hospitals Board fees will not increase this year. Jeanne Atherden, the Leader of the Opposition, said members of the public would be unhappy to see insurance costs increase. She also asked the Government for updates on programmes designed to improve health, such as the enhanced care programme for people with chronic, non-contagious conditions. Michael Dunkley, the Shadow Minister of National Security, called the monthly cost increase “significant for anyone”. Mr Dunkley said that the Progressive Labour Party’s General Election platform had pledged to reduce the cost of healthcare. He added: “One of the first things that’s happened is the cost of healthcare has increased because the cost of insurance has increased. Where are seniors going to find that extra $21?” The comment drew a point of order from David Burt, the Premier. He said: “FutureCare is not going up, so there is no increase in health insurance rates for seniors.” He added it was “incredibly rich” to hear concerns from opposition members about the cost increase. He added: “We are here because they received advice that they had to increase rates for utilization and they ignored it. “So, when I hear a former premier say that ‘We will support the tough decisions’, I have a very simple question — why didn’t you make them?” Patricia Gordon-Pamplin objected to Mr Burt’s statement. She said: “To hear the Premier say that we didn’t want to make the tough decisions is not just disingenuous, it’s completely misleading.” Ms Gordon-Pamplin added: “What I will not do is sit and listen to history be retold or reframed to suit the political narrative that the Premier wishes to advance.”
2018. June 28. The island’s health watchdog has launched a feedback survey that gives the public the opportunity to weigh in on its future. The survey will also help the Bermuda Health Council prioritize the problems facing health in Bermuda, determine its future direction and identify policy opportunities to improve health outcomes. Tawanna Wedderburn, the council’s chief executive, said: “The Health Council works hard to ensure the voice of the people is represented in healthcare. As we continue to monitor the high costs of health insurance and quality health services, it is crucial to collect valuable feedback about our mission and vision, for the future. To do this, we have created an easy to complete survey. We will release survey results to the public and use the information to guide our strategic direction over the next few years.” Everyone in Bermuda is asked to participate. The survey takes less than five minutes to complete.
2018. May 18. A partnership between a Bermuda charity and a US hospital group has delivered “cutting- edge” cancer treatment, a visiting expert said yesterday. Mark Davis, executive director of strategic initiatives and business development at Dana-Farber/Brigham and Women’s Cancer Centre, said that the treatment provided by Bermuda Cancer and Health Centre in partnership with his organisation represented the “shining example” of what was possible. Dr Davis said: “We have been able to provide truly cutting-edge care to people — people that would never have gotten it before, or people who might have gotten it but would have to spend a month or two away from their family and friends.” Dr Davis was speaking at a press event to mark the first anniversary of the radiation therapy unit at BCHC. Chris Fosker, radiation oncologist at BCHC, said the provision of radiation treatment on-island had been “hugely positive” for the care of people with cancer. Dr Fosker said: “It’s been an incredible team effort, and everyone who’s been involved has made a difference.” A memorandum of understanding between the two organisations was signed in 2015. Dr Fosker said that the collaboration between BCHC and DFBWCC delivered “world-class care”. He added: “Every single patient here has had personalized, world-leading radiation care.” Dr Fosker said the collaboration between BCHC and DFBWCC had sparked interest around the world, including the US, Canada, Australia and the Caribbean. Mr Davis said that any of the staff at DFBWCC, which provides cancer treatment at its 12 centres, would feel “absolutely comfortable” having family members treated at BCHC. He explained: “This is the cutting-edge level of care that we would all expect and hope for anybody in need.” Mr Davis added: “I point to this as the way that it should and could be done.” David Kozono, radiation oncologist at DFBWCC, said that he had treated a number of Bermuda residents for lung cancer in Boston before the radiation unit at BCHC opened. Dr Kozono added: “It’s clear looking at their eyes and talking with them how painful it is to be separated from family, friends and other loved ones for the six to seven weeks it takes to treat typical lung cancer. Being able to care for people right here in their neighborhood and in the company of people they know cannot be overstated.” A total of 130 patients have been treated at the radiation clinic free of charge. Treatment costs are covered by fundraising efforts, including the annual Relay for Life event which is to be held tonight and tomorrow. Judy White, president of the board of directors at BCHC, said that more than $2 million had been raised by the event over the past four years. Ms White added: “We urge Bermuda to continue to support these events as the money raised allows us to provide universal healthcare. No one will be turned away because they cannot afford to pay.”
2018. May 2. Dozens of people took part in a Bermuda Trade Union Congress march for workers’ rights with a focus on affordable, accessible healthcare yesterday. The BTUC recognized International Workers’ Day in the May Day march through Hamilton, starting at Victoria Park. BTUC president Jason Hayward said May Day recognized the achievements, fights and struggles of workers across the world. He continued: “Accessible and affordable healthcare in Bermuda is a concern. It is a theme because we simply do not have accessible and affordable healthcare in Bermuda. Brothers and sisters — our end game is universal healthcare coverage for all. Healthcare should be deemed to be a human right. Healthcare should not be viewed as a commodity.” The BTUC said the cost of Bermuda’s healthcare was alarming to all workers and their families, and implored all stakeholders to commit to finding solutions to Bermuda’s healthcare crisis. Mr Hayward said the Government should ensure that it had a proper health plan with appropriate regulation that sets reasonable healthcare costs for providers. “Providers need to ensure that they provide quality care and we also need our insurers to come on board. The premiums that Bermudians pay are simply unaffordable and so as a community we have to commit to work together to ensure that we reduce the healthcare costs in this country.” Mr Hayward said that the BTUC was advocating for a sustainable and improved healthcare system and for all stakeholders to work towards universal coverage in Bermuda, so that all residents have access to basic health insurance coverage, that healthcare coverage contributions are affordable and that all residents have access to healthcare services. The Progressive Labour Party joined the BTUC in recognizing International Workers’ Day with David Burt in attendance as well as his Cabinet. The Premier said: “The matter that is being brought before us is an important one. Healthcare is something that needs to be right and this government is committed to getting us to the place where we can afford healthcare.” Health minister Kim Wilson described the theme as “the most fundamental goal of my ministry and of our national health plan”. She added: “In the past week, I’ve met with over 120 health system partners and stakeholders to update them on the progress made and the next steps under the health plan. I stressed to everyone that affordable and accessible healthcare for all is the number one priority for me and we will bring about the reforms needed to make this happen. I want everyone to have access to preventive healthcare to avoid problems and resolve issues before they escalate.”
2018. April 24. The Bermuda Organ Donor Association appealed yesterday for the public to consider organ donation and to make their wishes clear to their families. The news came as the association greeted morning commuters at Crow Lane roundabout and encouraged them to sign up to give “the gift that keeps on living”. Kerry Brislane, the BODA treasurer, said: “Our message is pretty simple — we’d like people to have the conversation about what their wishes would be with their family members. The gift of organ donation is a tremendously generous thing to do, and the impact this can have on the recipients lives is definitely life-changing, and can be life-saving. If families have discussed and agreed on their wishes, it makes it so much easier if they are ever asked the question.” Dr Brislane, a hospital anaesthesiologist, was speaking as the island kicked off Organ Donor Week. She said statistics from the New England Donor Service showed that there had been 13 organ donors from Bermuda in the past decade. Donors ranged in age from 16 to 73 and a total of 24 kidneys, 13 livers, five hearts, eight lungs and three pancreas were donated. Dr Brislane said: “The only way to assert your wishes is on your driver’s licence, but ultimately your family will get to decide. We would like to see the Organ Donor Register formalized by the Government, as it is already in the legislature. This would mean people could sign up and be assured that their wishes will be adhered to. This takes a lot of pressure off families. Organ donation is the gift that keeps on living. In the words of Maya Angelou, ‘Be a rainbow in someone else’s cloud’.” The group will run radio interviews, information advertisements in The Royal Gazette and talk to the public to answer questions about the organ donation process. We decided to do the morning wave as it is a good way to reach a lot of people in an informal way and make them think, ‘hey, what is that all about?’ In recent years, we have been trying to find new ways of reaching a bigger audience and so we thought we’d try a popular Bermuda way. It was a lovely way to start our Monday with lots of smiles and waves and toots from the people coming passed.” She added: “We are hoping that after seeing us on the roundabout people might then be prompted to read and listen to the information provided.”
2018. March 28. Charity Age Concern is to bring back free health checks for members for a second year. The charity will host its first event today and there is still time to sign up. Anita Furbert, a registered nurse and Age Concern’s education officer, said: “We did three in total last year and this year we are taking the same route. “We didn’t want to do a one-off. We wanted to make this a staple for the community. We wanted to have health checks available at various points through the year so that people who had difficulties could go to these health checks. We found that a lot of members, a lot of participants, did not know their health status because they did not go to the doctor just to check on that. The health check was a way to give them information on their specific issues so that they can go more specifically to their private providers to have those things followed.” Age Concern members who attend will get a range of checks, including blood pressure, blood sugars and weight. Ms Furbert said: “We have a nutritionist or dietitian who will tell them about what those numbers mean.” There will also be eye checks, as well as dental screenings. Ms Furbert added: “And we have asthma and emphysema screening so, we have Open Airways with us. That’s new this year.” She explained that health professionals will be able to advise people on what steps to take at the end of their health check up. Ms Furbert said: “That’s the step that we want people to be engaged and involved in — making a difference for themselves. If they don’t have a doctor, we can refer them to the health clinics for their blood pressures and blood sugars and those kind of things and they can get referred from there.” Ms Furbert said the checks were also used to compile statistics on Bermuda’s senior population. But she emphasized that all information gathered is confidential. The first screening last year saw about 80 people take part. Ms Furbert said 40 people had signed up to this session, which will be held at insurance firm Chubb on Hamilton’s Woodbourne Avenue. She added that the deadline for registration is 2pm on Tuesday. The checks will run from 10am to 3pm. Shuttle services will run from Bulls Head and City Hall car parks from 9.30am to 2.30pm.
2018. March 27. A new diabetes centre will offer affordable medication and education under one roof, the Bermuda Diabetes Association said yesterday. Debbie Jones, executive director of the association, said the organisation was “acutely aware of the urgent need to improve our healthcare offerings and to make diabetes healthcare more accessible and affordable”. She was speaking after a 2017 report into patients with diabetes highlighted how chronically sick Bermudians fare worse in comparison with British diabetes patients. Local residents and health IT specialists Sean and Jenny Riddell commissioned the study, which they said “clearly shows Bermudian diabetics are not receiving the effective preventive care they should”. Ms Jones said “the first and foremost problem is that healthcare is so expensive”. She added: “To this end we have embarked on an ambitious project of purchasing and renovating a building which when completed will be the Hilton Hill Diabetes Centre. It will house our enhanced pharmacy, which provides medicine for those with diabetes at an affordable price, and our diabetes education centre under one roof. Bermuda is a small island and it should be possible to make this island of ours an example of what good affordable accessible healthcare is all about.” Ms Jones also backed the call for an island-wide electronic medical record system that would enable better monitoring — and risk assessment methods to identify at-risk patients before they got more ill. She said: “An electronic health record is so important in so many ways. Ms Jones added: “In the UK there are guidelines called the Nice guidelines. These guidelines dictate what standard care patients should expect to receive and based on what is actually delivered to patients provides the basis for what physicians will be paid. Physicians have to fill out records of that visit in order to receive payment. However, that is the NHS and Bermuda is private but there should be some reporting mechanism in place that indicates whether the person with diabetes has received the standard of care.” Ms Jones said standards of diabetes care were revised each year by organisations such as the American Diabetes Association, Diabetes UK and Diabetes Canada. She added: “For example if a patient smokes and we know that smoking and diabetes is a ‘double whammy’ that patient should be sent to smoking cessation classes. That referral would be part of the electronic record. Similarly a newly diagnosed patient with type 2 diabetes should be sent for diabetes education and dietary advice. The electronic health record would provide the mechanism for monitoring. An electronic record had been talked about for years but “certain sectors” were reluctant to go ahead with it. The Bermuda Diabetes Association tried to introduce a diabetes electronic record years ago and the cost of implementation was given as the reason physicians’ offices were reluctant to do it. Legislation could and should alleviate that burden.” Diabetes educator Sara McKittrick added that the report raised the issue that current structure does not reward GP practices for prevention and education which is grossly undervalued. “This all becomes very relevant when we look at current healthcare costs being so high while not achieving the desired health outcomes that we could expect when it comes to diabetes management,” she said.
2018. March 20. A grant paid to two healthcare clinics in the wake of cuts in fees for MRI and CT medical scans was funded through a vacant post, the Senate heard yesterday. Progressive Labour Party senator Crystal Caesar said no extra money was paid to the health ministry to fund the $778,000 payment to the Brown-Darrell Clinic and Bermuda Healthcare Services. She said: “No projects were put on hold in order to give this grant and the funding was from a vacant post, so the money was found within the health budget elsewhere. I think we are trying to make a narrative which is not correct. It’s not that these are additional monies that could have gone somewhere else. These monies had been budgeted. They were moved from one area that would not have been used otherwise to rectify this particular situation.” Ms Caesar was not able to say which post the funds came from. She was speaking after One Bermuda Alliance senators Andrew Simons and Justin Matthias raised questions about the grant during the Budget debate on health. Mr Simons said: “That number of $778,000 is larger than all of the other grants except for the grant to the Lady Cubitt Compassionate Association. It is an enormous amount of money to have been doled out.” He added: “Surely, $778,000 could have been spent on nurses, dentists, technical officers — there is a cost to that grant in services that were not rendered to enhance public health.” Ms Caesar defended the Government’s decision and pointed out that $1.8 million was paid to Bermuda Hospitals Board, which was also affected by the fee cuts. “The fact of the matter is that both of these entities, the hospital and the Brown-Darrell Clinic provide a very essential service for the Bermuda community as a whole. Because the fees in a particular area were decreased, which did not make either entity viable in those particular areas, a grant was determined and given, not through a supplemental, to these entities so that they could continue to service the Bermuda community.” She added: “The $778,000 is for June 1 to March 31 of 2018. There was no supplementary required for this.” The Government was asked yesterday what post the cash came from, but there was no reply by the time of press. Ms Caesar added that a $100,000 allocation in the grants for the fiscal year 2018/19 was a “place holder” that had not been earmarked for the Brown-Darrell Clinic. The Bermuda Health Council reduced the fees that could be charged for MRI and CT scans last year. Ewart Brown, the former premier and owner of the Brown-Darrell Clinic, said the cuts left the business unsustainable and the CT unit was shut on January 31. Ms Caesar also announced that new health insurance rates and medical fees would not be ready by April 1 and would instead be implemented by June 1. She said: “This is due to the long-needed conversion of the BHB fees to a rational methodology to standardize fee levels at an internationally accepted standard, based on the relative value of procedures. We are undertaking this initiative as we speak.” Ms Caesar added: “I can advise at this time, however, that while the impact of the new relative value unit or RVU fee structure, will be revenue neutral for BHB, we anticipate an increase to the standard premium rate due to continued increases in utilization of hospital services.” Mr Simons said: “That really undermines the argument that was used earlier this year that we should have used that methodology, if it’s not ready now.”
2018. March 12. The cost of the Bermuda Government’s lawsuit against American-based medical group Lahey could reach $4 million, a former attorney-general has warned. Progressive Labour Party MP Michael Scott, a lawyer with legal practice Browne, Scott, told Parliament on Friday that costs had already topped $3 million. He was speaking after Kathy Lynn Simmons, the Attorney-General, announced that the lawsuit, which alleged that Lahey conspired with Ewart Brown, a former premier, to defraud the island of millions of dollars in healthcare charges, had been dismissed by a United States judge. Ms Simmons, who signaled the Government would not pursue the case any further, said that although the cost of the case had not been assessed, it had run up a bill of “well over $1 million”. But Mr Scott said: “I have taken time to research and ask questions of my colleagues as to what we have paid to a law firm called Cooley LLP.” He added that Trevor Moniz, then One Bermuda Alliance Attorney-General, approved more than $3 million for the Boston law firm. Mr Scott said: “It is bound to reach $4 million. How much could we have done with $4 million?” He added that the dismissal confirmed the view that the case was “a strategically and politically motivated suit aimed at harming black leadership in this country in general, and in particular aimed at harming the Progressive Labour Party pre the General Election”. During Friday’s motion to adjourn, Moniz, the Shadow Attorney-General, was kicked out of the House of Assembly amid a row over the files connected to the case as the dismissal on technical grounds of the Government’s legal action against the Boston clinic in a US court dominated proceedings. Zane DeSilva, a PLP backbencher, said the lawsuit was a “personal, racist vendetta against Dr Brown”. He added that the OBA had an “endless pocket of money for witch-hunts” and that “today, we saw where a lot of that money went — down the drain”. PLP backbencher Derrick Burgess said: “These guys really want to kill this man. That’s the objective of it. This country needs to leave Dr Ewart Brown alone. He’s done a lot for this country.” Jamahl Simmons, economic development and tourism minister, added that the people of Bermuda had to pay for this “cockamamie revenge scheme”. Shadow government reform minister Michael Dunkley, who was the Premier at the time the case was filed, said he would not “run from decisions or actions that were taken”. He added: “As the Premier at the time, I’m willing to take all the flak from members on that side and the people of Bermuda for decisions we made. But, Mr Speaker, I can assure you, that we made decisions which at the time we thought in the best interest of moving this country forward.” OBA MP Patricia Gordon-Pamplin added: “I take responsibility for actions for which I am responsible. Because I take responsibility, I don’t just read one excerpt from something and assume that it is the whole. If we get to a stage in which there is full disclosure, and that disclosure dictates something that would indicate that I have made a decision collectively with my colleagues which was wrong, I am woman enough to stand and say so.” But David Burt, the Premier, said: “The former government could not find it within them to put the country’s interests ahead of their own narrow political self-interests.”
2018. March 10. The lawsuit undertaken by the former One Bermuda Alliance government against the Lahey Clinic put Bermuda’s treaty relationship with the United States at risk, the Speaker of the House said last night. Dennis Lister said: “Our treaty relationship was in threat based on what I have in front of me.” Mr Lister’s statement came after reading an e-mail he was presented by David Burt, the Premier, during the Motion to Adjourn in the House of Assembly. Mr Burt had sought to read the e-mail during his address to Parliament. But Mr Lister warned Mr Burt against reading the letter. He explained: “If it’s sensitive, I don’t think it should be made public.” Mr Lister said he would read the last line from the e-mail. He read: “This is a very important matter which can have an impact on our treaty relationship. I am available to speak with you at your convenience. And it’s singed by the individual.” Mr Lister said that he would not read the full content of the e-mail nor identify the persons named. But Mr Lister said: “It did come from a senior officer in the US Criminal Justice Department.” He said the email was addressed to former Attorney-General Trevor Moniz’s chambers.
2018. March 10. Shadow Attorney-General Trevor Moniz was kicked out of the House of Assembly last night amid a row over files regarding the Bermuda Government’s lawsuit against the Lahey Clinic. He was told to leave after he repeatedly accused national security minister Wayne Caines of “misleading the House” and after Dennis Lister, the Speaker of the House, warned him that he would have to leave if he continued “his game”. Mr Moniz responded: “Well, that’s fine, Mr Speaker.” Mr Lister then told him to walk. The dismissal of the Government’s case against the Boston clinic in a US court on technical grounds dominated last night’s Motion to Adjourn. The row broke out after Mr Caines said the Attorney-General, Kathy Lynn Simmons, had to deal with not having all the case files, as well as “allegations of documents being shredded”. Mr Moniz, on a point of order, insisted that the files were all with the law firm. Mr Caines responded: “Why would any government minister, why would anyone in charge of justice have files outside of a government office? What type of country do we live in when we do not have files where they can be checked, where they can be managed, where they can be looked at?” But Mr Moniz said: “The case was in Massachusetts. Wouldn’t the files be in Massachusetts — that’s where the case is.” In response to Mr Caines stating that there should always be copies of files kept in the country, Mr Moniz again insisted that he was “misleading the house” and that the files were always available. Mr Lister said: “I think you’ve stretched your point.” Mr Moniz responded: “Let me finish, Mr Speaker.” Mr Lister said: “Member, you continue your game and that door is going to be yours.” Mr Moniz said: “Well, that’s fine, Mr Speaker.” After his ejection, PLP MP Michael Scott accused Mr Moniz of deliberately getting himself thrown out of the Lower House. Mr Scott said: “That Member, the chief law officer, has by calculation and device arranged for his self-ejectment from the house so that he does not have to answer.” He added that Mr Moniz’s actions told “a thousand tales of the absence of accountability”. The heated debate came after Mr Moniz said in a statement earlier last night that he was disappointed that the Government’s case was thrown out on technical grounds. Mr Moniz defended his decision to launch the case last year and said Judge Indira Talwani’s statement suggested criminal acts may have been committed. Judge Talwani said in her ruling: “It may well be that Bermuda’s allegations as to Lahey’s commission of various predicate acts would suffice for criminal charges … or civil enforcement proceedings brought by the US Attorney-General.” Mr Moniz added: “In other words, the federal judge is saying that criminal acts may have been committed. She pointedly noted that American institutions such as Johns Hopkins may have a valid domestic injury claim against Lahey within the US.” Kathy Lynn Simmons, the Attorney-General, said yesterday that the case would not be pursued in Bermuda. The case was dropped because the judge found that Bermuda had suffered no loss in the US. Mr Moniz said the US Supreme Court had narrowed its legal test after the Lahey investigation had started. He added: “The dismissal of the Government’s civil case against Lahey Clinic comes as a disappointment. As Attorney-General, I made the decision to issue proceeding following an exhaustive investigation. Throughout the entire process, I acted on the basis of legal advice and in the best interests of the community. Ultimately, the case was dismissed on a technical ground, namely that there is insufficient domestic injury in the US to bring a case before the American courts. This is a fast-moving area of the law, with the US Supreme Court only deciding to narrow the relevant legal test in the summer of 2016, well after the investigation into Lahey’s affairs began. A further appeal would be needed to clarify this point. It is important to point out that the case was based on compelling evidence and that the complaint was meticulously well-sourced — in many instances, with the very words of those involved.”
2018. March 9. A United States judge has dismissed a case against American-based medical group Lahey that alleged it conspired with Ewart Brown, the former premier, to defraud the island of millions of dollars in healthcare charges. “From our perspective, the case is closed, and we do not intend to pursue it any further,” Kathy Simmons, the Attorney-General, said this afternoon. The Attorney-General’s remarks came in the wake of the decision by Judge Indira Talwani of the US District Court in Massachusetts allowing Lahey’s motion to dismiss. The ruling, made on Thursday, was “exactly what I had anticipated from the beginning”, Ms Simmons said. The Government opted to pursue the matter “given the politically charged nature” of the case, she added, saying it had been important for the decision to come from “an independent assessor”. No final cost for the case has been tallied, but Ms Simmons said it had run up costs “well over $1 million”. The Lahey Clinic responded by issuing the following statement: “Lahey Hospital & Medical Center has a 25 year track record of caring for the people of Bermuda while maintaining the highest ethical standards for all business relationships. We were confident that the claims made in the suit were baseless and are pleased with this dismissal. Our team of physicians looks forward to continuing to improve the health of Bermuda residents, create programs to address significant public health issues and provide the care the people of Bermuda need and deserve.” In her decision, Judge Talwani said that a claim under the federal American Racketeer Influenced and Corrupt Organisations Act could not be considered because Bermuda had suffered no loss in the US. Judge Talwani said in her ruling: “Bermuda has not shown that it suffered any injuries in the United States as a result of the alleged scanning scheme. Without such an injury, Bermuda’s RICO claims as to the scanning scheme arise out of extraterritorial injuries and must be dismissed.” Another claim for damages over the FutureCare insurance plan was also dismissed because it was nothing to do with the US. Judge Talwani said: “The Kurron Bermuda project involved developing the ‘FutureCare’ public insurance plan. Bermuda alleges that ‘Brown used his influence and connections to ensure that Lahey was favored over other potential US healthcare providers, including Johns Hopkins, for lucrative contracts relating to ‘FutureCare’.” But she added: “As FutureCare is a Bermudian public insurer which reimburses healthcare costs of Bermudian residents, the court cannot, without more, find any injury from these contracts to business or property in the United States. While entities like Johns Hopkins, whose domestic profits were competitively injured by such contracts, might have a valid domestic injury claim, Bermuda does not.” The judge added: “The question presented in this case is whether Bermuda may bring an action for the various injuries alleged under RICO’S private right of action. It may well be that Bermuda’s allegations as to Lahey’s commission of various predicate acts would suffice for criminal charges ... or civil enforcement proceedings brought by the Attorney General ... however, the focus of this motion is whether Bermuda, as a private party, may bring these charges. That depends on whether Bermuda has alleged domestic injuries to business or property caused by Lahey’s conduct. The injuries in this case are assessed in turn.” Judge Talwani added: “Bermuda also brings claims under Massachusetts General Laws c. 93A, § 11 for unfair business practices and common law claims under theories of unjust enrichment, civil conspiracy, and fraud. Given the early stage of this litigation and the fact that the parties have not yet begun the arduous task of discovery, retaining jurisdiction over Bermuda’s pendent state law claims would not serve such interests. Accordingly, Bermuda’s state-law claims are dismissed without prejudice.” The case, started under the former One Bermuda Alliance Government, claimed Dr Brown, the owner of Bermuda Healthcare Services and the Brown-Darrell Clinic, used his position as a Government minister to promote Lahey’s interests in Bermuda and the hospital paid him “bribes disguised as consulting fees”. It was alleged the arrangement led to Lahey gaining contracts with King Edward VII Memorial Hospital and to it becoming the “service provider of choice for Bermudians, both on the island and in the United States”. The civil suit also claimed Dr Brown’s clinics in Paget and Smith’s conducted “excessive, medically unnecessary and frankly dangerous scans” in order to increase payments received from health insurers. The claim also alleged that Dr Brown paid Lahey a portion of the reimbursement for reading each scan, making the hospital millions of dollars and that Lahey “stayed silent” about the “extreme level of unnecessary and possibly dangerous scans” because it was “blinded by its desire to keep its ‘consulting’ relationship with Dr Brown intact”. Other allegations included that Dr Brown and his “surrogates” successfully pressured government officials to increase the remuneration paid for tests and that he “offered and paid kickbacks” to island doctors, disguised as commissions, to refer patients for scans to his clinics. The Government submission to the court said that the level of testing conducted at Dr Brown’s clinics led to Bermudians becoming “among the most scanned patients in the world”. Reacting in a statement today, former Attorney-General Trevor Moniz said: “The dismissal of the Government’s civil case against Lahey Clinic comes as a disappointment. As Attorney-General, I made the decision to issue proceeding following an exhaustive investigation. Throughout the entire process, I acted on the basis of legal advice and in the best interests of the community. Ultimately, the case was dismissed on a technical ground, namely that there is insufficient domestic injury in the US to bring a case before the American Courts. This is a fast-moving area of the law, with the US Supreme Court only deciding to narrow the relevant legal test in the summer of 2016 – well after the investigation into Lahey’s affairs began. A further appeal would be needed to clarify this point. It is important to point out that the case was based on compelling evidence, and that the complaint was meticulously well-sourced – in many instances, with the very words of those involved.” He noted Judge Talwani had not discounted the possibility criminal activity took place, adding: “The federal judge is saying that criminal acts may have been committed. She pointedly noted that American institutions such as Johns Hopkins may have a valid domestic injury claim against Lahey within the US. Finally, it was a great blow to the case that members of the former Opposition, including the present Premier and Deputy Premier, filed objections to the case proceeding.”
2018. March 8. Hospital fees are to be adjusted in a move that will raise some costs and lower others, the health minister told the House of Assembly yesterday. Kim Wilson told MPs the changes will be “revenue-neutral to the hospital” and said the relative value method used was a “rational system” in line with reviews. Ms Wilson said: “At present some BHB fees are priced higher than international benchmarks, while others are priced much lower. “The intent is to remove this discrepancy by applying a rational, internationally accepted standard to set BHB’s [Bermuda Hospitals Board] fees. The purpose of this change is as a first step to deliver on the Government’s promise to review healthcare costs, which, in the long term, will allow us to contain insurance premiums. At present we know how much we are spending overall — $701 million in total, or just over $11 thousand per person, are the most recent figures. But we don’t know if we are spending it wisely, or whether we are paying fairly. To enable us to understand truly what we are spending on, measure whether we are spending it properly, we need a rational fee system.” Ms Wilson added that the relative value method would “move us in the right direction, and provide us a stronger foundation for evaluating our services and programmes”. The same relative-value scale has already been introduced for diagnostic imaging, where fees for procedures like mammographies went up while others, like X-rays, went down.
2018. March 5. Parliament has approved legislation to update the regulation of psychologists. The Psychological Practitioners Amendment Act 2018 replaces 20-year-old legislation governing the profession. Anyone not registered in Bermuda will now be prohibited from practising as a psychologist. Practitioners also have to get indemnity insurance against claims of negligence and malpractice. The updates were made in consultation with the Bermuda Psychologists Registration Council, which will become the Bermuda Psychologists Council. Jeanne Atherden, the Leader of the Opposition, and shadow health minister Susan Jackson backed the legislation. Tinée Furbert of the Progressive Labour Party said the updates were “succinct as regards psychology”.
2018. February 27. New hi-tech computerized heart scans will help cut the risk of heart disease, the Bermuda Hospitals Board has said. The scans can detect calcium deposits and other obstructions in blood vessels which can lead to blockages and heart problems. Dr Joseph Yammine, BHB consultant cardiologist and director of the programme, and Dr Anders Hauggaard, a consultant radiologist who has used the technology in previous posts in Sweden and the Arabian Gulf, set up the programme. A joint statement from Dr Yammine and Dr Hauggaard said: “This programme, where we provide calcium scoring for cardiac risk screening and coronary angiography for assessment of coronary disease and overall heart conditions, is of great value to the community. It is particularly important because Bermuda does not have a cardiac catheterization laboratory. This programme offers an alternative in many cases to surgery to get a clear picture of the state of the vessels in and around the heart and may result in less referrals to facilities overseas.” The new tests available are CT angiography and cardiac calcium scoring. In CT angiography, 3D images of arteries that supply blood to the heart are taken with a CT scanner. The test can help diagnose the cause of chest pain and may indicate blockages in these vessels and conditions like atherosclerosis — fatty deposits in blood vessels. The programme started earlier this month to coincide with Heart Month and about 15 people have used the service so far. Radiology technicians with special training and experienced nurses perform the tests under the supervision of a doctor. Dr Sam Mir, BHB director of cardiology, said: “This programme can be a significant benefit to improve the care of our cardiac patients in Bermuda where heart disease remains the number one killer.” Dr Daniel Stovell, BHB chief of radiology, said: “This testing is carried out with minimal exposure to radiation. We have paid close attention to this and are pleased with the achievement in the pilot phase of the programme which took place earlier this month.”
2018. February 23. Kurron Shares of America first made headlines in Bermuda in March 2003 when it was hired to conduct a study of King Edward VII Memorial Hospital and what was St Brendan’s Hospital, now the Mid-Atlantic Wellness Institute. Nelson Bascome, then health minister, announced the appointment of the health management and consultancy firm, whose headquarters were in Manhattan, which sparked opposition criticism that it had come “out of the blue”. The firm was paid $450,000 for a report on the two hospitals, according to parliamentary answers, but a far bigger payday was on the horizon for Kurron. In 2007, the company won a five-year, $13.5 million contract to help the Bermuda Hospitals Board to develop a long-term healthcare strategy for the island, which beat a bid by better-known Johns Hopkins Medicine International. The decision caused criticism by doctors, who branded Kurron Shares as “minor league”, and claims that Dr Brown had insisted on the appointment against the wishes of the hospitals board. Kurron had donated $10,000 to a foundation set up by Dr Brown’s wife, Wanda Henton Brown, the previous year to offset the price of expensive tourism events on the island. Mrs Brown and Kurron’s chairman and chief executive Corbett Price, according to US media reports, had been friends and business associates since at least the 1990s. When Kurron’s donation to the Tourism Helps Everybody Foundation, and donations to the foundation by other non-Bermudian companies who gained government contracts, were mentioned by Opposition MP Grant Gibbons in the House of Assembly, Dr Brown branded Dr Gibbons a “racist dog”. Kurron set up an island firm, Kurron Bermuda, in 2007. The company got permission from Derrick Burgess, when acting finance minister, for its entire share capital to be allotted to Mr Price and his son, Devin Price, both non-Bermudians, according to documents available at the Registrar of Companies. Kurron Bermuda was dissolved by the Registrar of Companies in 2016 because it was no longer active. Kurron’s contract with the BHB was terminated by Paula Cox in 2011 — a year and a half early — after she succeeded Dr Brown as premier. Kurron, which also won a contract with the Ministry of Health to develop the FutureCare health insurance scheme for seniors, appears to no longer exist. The company website still lists the Bermuda Hospitals Board and government agencies in Bermuda as “current engagements”, but the company’s listed phone number is out of service and US news reports suggest it closed its headquarters in Manhattan in 2011. In 2013, a WNYC News article described Kurron and Mr Price as having “cut a trail of financial and medical mismanagement, run-ins with regulators and public controversies”. A BHB spokeswoman said yesterday: “BHB does not have a contract with Kurron and has had no association with the company since the last contract was terminated in 2011.” Mr Price on social media said he is chairman and CEO of Quantix Health Capital, but Quantix’s phone number is also out of service and e-mails to the company bounced back.
2018. February 23. A controversial multimillion-dollar healthcare contract axed by former premier Paula Cox is back in the spotlight in the Government’s lawsuit against the Lahey Clinic. Lawyers involved in the civil case are examining the deal that Kurron Shares of America landed with the Bermuda Hospitals Board during the premiership of Ewart Brown, who is named as Lahey’s co-conspirator in the lawsuit. The Royal Gazette understands that before the change in government last July, the One Bermuda Alliance administration had considered filing a similar lawsuit against Kurron, based on e-mails between the Maryland-incorporated company and Dr Brown. The Cabinet is believed to have decided against the move before the General Election, which the Progressive Labour Party won with a massive majority. It is not known if the new PLP administration plans to take legal action in connection with Kurron. Attorney-General Kathy Lynn Simmons did not respond to a request for comment yesterday. Kurron, led by American businessman Corbett Price, won a contract with the Bermuda Hospitals Board in May 2007. The company got the business despite opposition allegations of cronyism leveled against Dr Brown, who was then the premier. The contract was terminated 18 months early by Ms Cox, after she succeeded Dr Brown as premier. The deal is now being re-examined because of claims in the Government’s lawsuit for unspecified damages against Lahey for an alleged conspiracy with Dr Brown to defraud the public purse. A key allegation made by the Government is that Lahey bribed Dr Brown, when he was premier, in order to win Bermuda contracts and other work. It is alleged “rigging” of the bidding system took place, which prevented the island from getting the best services or best prices. Dr Brown and Lahey deny the allegations. The lawsuit also alleged: “In 2007, Dr Brown secured a $13.5 million, five-year contract to develop a long-term healthcare strategy for the island for an American-based healthcare management and consulting company known as Kurron Shares of America.” It said Mr Price was a former business associate of Dr Brown’s wife and claimed Dr Brown “knew he could control Mr Price and get him to work with Lahey”. The claim added: “As part of the project, various contracts would be awarded to medical partners, including Lahey, to re-imagine and revamp King Edward VII Memorial Hospital. Dr Brown ensured that Kurron obtained this contract by silencing opponents to Kurron’s selection and removing them from the Bermuda Hospitals Board.” It is alleged that Dr Brown “facilitated” the appointment to BHB of Wendell Hollis, “his personal lawyer and confidante, who was also Kurron’s lawyer, thus paving the way for the award to Kurron”. The complaint includes an e-mail allegedly sent from Dr Brown to a Lahey executive, which told her to let Kurron bid for the hospital contract with the promise that “Lahey’s interests will be protected”. Dr Brown told the Lahey executive in another e-mail that Kurron had won the contract before the news became public knowledge. The Government’s claim said: “Dr Brown followed through on his promise that Lahey would receive work from Kurron. In July 2007, he publicly announced a new partnership between KEMH and Lahey.” The Kurron contract was discussed at a court hearing last month in Boston. Judge Indira Talwani heard a motion from Lahey to have the Government’s complaint against it dismissed. The judge has yet to deliver a judgment on the motion. Elizabeth Trafton, lawyer for the Government, referred to the Kurron contract as she outlined Lahey’s alleged “rigging of the bidding process” for contracts. Terence Lynam, counsel for Lahey, said: “The allegation is simply that Dr Brown told Lahey that Kurron won the contract. And that became a matter of public knowledge. I don’t see how that is a corrupt act.” He added: “There’s no allegation that Lahey benefited in any way from the fact that Kurron got a contract. That’s one allegation that they make, but it doesn’t go anywhere.” Mr Lynam said: “It’s really important ... in a case involving bribery under the Foreign Corrupt Practices Act to allege some official acts with some particularity. “What is it that Dr Brown did in his capacity as a government official, as opposed to his capacity as a practising physician?” The lawyer added: “Lahey never got anything from a contract that Kurron got. It never led to Lahey getting anything.” Dr Brown told The Royal Gazette this week: “I do not have, and have never had, a business relationship with Kurron. The owner, Corbett Price, has been a friend for many years. I met him after he began working for BHB.” Mr Hollis, who served as deputy chairman of the BHB between 2007 and 2012, told The Royal Gazette last year he “barely knew Ewart Brown” when he was appointed deputy chairman. He added that he “didn’t become his lawyer until long after my five years was up on the BHB”. Mr Hollis represented Dr Brown in July 2009, when the PLP politician threatened legal action against Kim Swan, then the Opposition leader. Mr Hollis said in an e-mail yesterday the matters involved were about ten years old. He wrote: “I am not interested in getting into a ‘who said what to whom when’ debate about matters which took place so long ago and for which memories are now fading.” Mr Price could not be contacted for comment.
2018. February 23. Spending on healthcare is not the same as investing in health, the Bermuda Health Council has warned. The watchdog said more money should be spent on the social causes of poor health after David Burt, the Premier and Minister of Finance, said Bermuda had to be more selective in its healthcare spending. A spokeswoman for the BHeC said: “The $700 million that we spend on healthcare is significant. However, within the scheme of that spend, we have not invested enough on social and economic policies that are shown to impact health. Investing in health is more than spending money in the operating room, urgent care centre, overseas hospital or pharmacy. To spend wisely, we must invest in the social determinants of health and find ways to get more value out of the healthcare dollars we spend. For example, to reduce high blood pressure, we should consider causes of social stress and have options to provide the public with access to affordable options of health prevention and promotion to reduce the causes of those stressors.” The BHeC spokeswoman said health cash had to be better targeted to improve the system for better long-term results. She added: “The amount of money invested should be related to specific health system and population health objectives. To be efficient in getting exceptional healthcare, we need to use available research and learn from the mistakes and successes throughout the world. It is also important to allocate resources to support our health system in becoming more progressive and innovative in the face of ever-changing global medical standards. We, in Bermuda, due to our size and expertise of providers, have a unique opportunity to reform our system and become a model jurisdiction for others to follow.” She was speaking in the wake of Mr Burt’s Budget announcement of a $27.3 million increase in health spending. Mr Burt said the extra cash would be used “to reinstate the Bermuda Hospitals Board subsidy budget and to provide long-term care and health services”. He added that the $700 million a year spent on healthcare was a “continued source of concern” and pledged the Government would reform the system. “There is enough funding in our health system to give all our residents the healthcare they need, but we must be much wiser about how we utilize these funds.” He also announced that a sugar tax on some items would be finalized after the health ministry’s consultation ended on March 1 and that the Government would reduce or scrap duty on a selection of healthy food items. The BHeC spokeswoman said sugar taxes would not fix the island’s health problems, but could “be a powerful tool towards cultural change”. She added that similar taxes had been used abroad to tackle poor nutrition and could also provide governments with extra money to subsidize healthier foods or health education. “Ultimately, the research shows that consuming better foods leads to better health.” The health council would hold talks on health system reforms over the next year.
An investment and solutions wish list
2018. February 13. The Bermuda Government may roll back steep cuts made to medical imaging fees which were blamed last month for the closure of a private scanning clinic. However, last night the Opposition hit back at claims that the One Bermuda Alliance administration had “ignored” technical advice and singled out diagnostic imaging for sharper fee cuts than those suggested. The reductions, recommended by the Bermuda Health Council, were decried last month by Ewart Brown, the former premier, who runs two private clinics offering medical scans. The CT scan unit at his Brown-Darrell clinic in Smith’s, which provided computer-processed X-ray imaging, was shut on January 31 after Dr Brown said the cuts left the business unsustainable. The possibility of fee cuts being partially reversed emerged in Friday’s House of Assembly, when OBA MP Trevor Moniz asked Kim Wilson, the Minister of Health, whether there was “any intention of changing the fees going forward”. In response, Ms Wilson said that three independent reviews before June 2017 had suggested relative value methodology as a technique for calculating medical fees. She added: “That’s the internally accepted methodology used in the US, Canada, Europe, the UK. It places a logical, rational and transparent fee structure on healthcare to assist in containing the cost.” She said the OBA administration had disregarded recommendations from the Bermuda Health Council, telling the House: “The former government ignored that technical advice and decided to apply fees that were much lower than what was being provided for, with respect to the relative value units provided by the technical officers of the Bermuda Health Council. I can say that this government is committed to reducing healthcare costs. We will be applying the relative values going forward, starting with the Bermuda Hospitals Board.” MPs also heard that the BHB, along with Dr Brown’s clinics, have each received payments directly from Ministry of Health funds, to compensate them for their lost earnings. Ms Wilson said that after an agreement was reached on December 8, 2017, a payment of $120,000 had been settled for Brown-Darrell Clinic, and $480,000 for Dr Brown’s other business, Bermuda Healthcare Services. The BHB’s payment is still being calculated based on levels of use, and Ms Wilson said she would not know that amount until the end of March. Opposition leader Jeanne Atherden responded last night: “Ms Wilson’s statement is misleading. The previous administration did not ignore technical advice from the Bermuda Health Council. The council’s diagnostic imaging fee schedule used the relative value methodology with a conversion factor of 83.8.” Every type of diagnostic imaging service comes with a specific code, with a conversion factor used to calculate the dollar value of a fee. The same conversion factor was applied to all diagnostic imaging services, Ms Atherden said. The former health minister added: “It was that fee schedule that was suggested to the minister, accepted, and passed by the legislature.” Ms Wilson was unavailable for comment yesterday — but Mr Moniz said he had asked the question in Parliament because “I just want these things to be out in the open”. He said he had asked the minister whether the Progressive Labour Party administration had been threatened with legal action. Ms Wilson responded: “Prior to this agreement being settled on December 8, 2017, there were discussions taking place between the Government and the Attorney-General.” Speaking to The Royal Gazette, Mr Moniz said: “The public is entitled to more information about what discussions took place, and how these numbers were arrived at, and why they’re paying this amount of money. Either they negotiated and arrived at an agreement or they didn’t. What I would like to know is, did [Dr Brown] have leverage on them?” Contacted last night for comment, Dr Brown responded: “There were absolutely no negotiations between myself and the Government concerning the fees. The Government told us exactly what the minister told the House.” Asked if he had been informed of any potential raising of imaging fees, and whether that might salvage his CT unit, Dr Brown said: “No, I have not.”
2018. February 6. Doctors from a top US hospital have helped island practitioners to keep up with the latest developments in heart and kidney treatment. The team from New York-Presbyterian Hospital held a seminar organized by the Bermuda Heart Foundation and sponsored by Colonial Insurance. Christopher Irobunda, a cardiologist at the New York hospital, said: “It’s about bringing up to date their awareness of cardiovascular disease and its impact on society. “That is one of the main reasons why we are here to support the Bermuda Heart Foundation and the Core Health Centre.” Dr Irobunda said one of the main reasons for the event was to highlight advances in the identification of cardiovascular disease. He said: “It’s about identifying these risks and educating the public. With advances in identification of risks comes the opportunity to treat. We have a lot of things that can be offered at New York-Presbyterian for the management of cardiovascular disease. In all those areas, there have been a lot of advances, both in the classic way to do it and the more recent, more minimally invasive ways to do it.” Dr Irobunda added that his hospital was happy to work with the BHF and the Core Health Centre. He said: “What’s exciting about us being here with Core is that it is a place that has the opportunity to identify these patients, offer them a way to follow up, and from there identify patients that have had cardiovascular disease and serve as a rehab place for them.” Simone Barton, executive director of the BHF, said it was important to highlight heart disease prevention. She said: “The world is affected by many diseases that are incurable, that you can’t do anything about. Heart disease is not one of them. One of the greatest benefits you can have in managing heart disease is getting out in front of it. If we can get out of disease before it happens, and we have partnerships with insurers like Colonial and experts like NYP at our side, we can prevent so many diseases from happening. We can stop heart attacks from happening.” Devid Serur, a US kidney specialist, said his focus for the seminar was on treatment options for end-stage renal failure. Dr Serur said: “Kidney disease often goes along with cardiovascular disease, often goes with diabetes and high blood pressure and kidney disease is on the rise. Because diabetes is more rampant than it used to be, hypertension is more rampant, and the population is ageing, these things combine to give you a higher rate of kidney disease. Some kidney patients don’t know that there are good treatments for the end stage of renal disease.” He said advances have been made in live-donor kidney transplants to make donor recovery easier and make transplants more available. “When you want to donate a kidney but are not compatible, we now have a kidney-pairing system where we can criss-cross pairs. We recently started another advance where people can donate a kidney to a loved one in advance of the loved one requiring it. We had a case of a grandfather who wanted to donate a kidney to his grandchild — the grandson does not require a kidney yet but he will in the future based on their kidney disease. The grandfather, feeling he might be too old to donate a kidney in ten years, donates a kidney now to someone else and ten years from now a voucher will be redeemed on behalf of that kid.”
2018. January 20. Specialists in heart and lung problems are to visit the island this month. Ofer Sagiv, an expert in heart medicine, will be at Northshore Medical & Aesthetics Centre from January 27 to 29, and Maciej Walczyszyn, who specializes in lung and critical care medicine, will be at the practice from January 26 to 29. Dr Sagiv is a vascular cardiologist in Connecticut, and is affiliated with multiple hospitals in the area, including the University of Connecticut Health Centre, John Dempsey Hospital and Yale-New Haven Hospital. He received his medical degree from Ben-Gurion University of the Negev. Dr Walczyszyn is a pulmonary and critical care medicine board-certified physician. He received his degree from Poznan University of Medical Science in Poland and is director of the pulmonary and critical care medicine division at Flushing Hospital Medical Centre. Dr Sagiv will see patients with shortness of breath, oedema, chest pain, palpitations, history of heart failure, heart attack or stoke, peripheral arterial disease and non-healing wounds of the lower extremities. Dr Walczyszyn will see patients with asthma, chronic obstructive pulmonary disease, emphysema, bronchitis or bronchiectasis, chronic cough, interstitial lung disease, pulmonary fibrosis, pulmonary hypertension, pulmonary embolism, sleep apnoea and lung cancer. Both doctors will only see patients by referral. For more information, contact Northshore Medical & Aesthetics Centre on 293-5476.
2018. January 20. A total of 15 cases of cervical cancer were reported in Bermuda last year, a Department of Health spokeswoman revealed last night. The news came as the Bermuda Cancer and Health Centre asked women to get screened for the disease and reminded parents to make sure their children are vaccinated against the Human Papilloma Virus, which can cause cervical cancer. The health department spokeswoman said: “There were 15 reported cases of cervical cancer in Bermuda last year and six reported cases of mouth, throat, oesophagus and nasal cancer related to the HPV virus. Cervical cancer screening by way of a Pap smear is a way to prevent cervical cancer. Women should be aware of this and understand the difference between screening for cervical cancer and screening for sexually transmitted infections.” Azuree Williams, BCHC education co-ordinator, added: “We are really looking at women taking better care of their health because cervical cancer is preventable, based on women getting regular screenings. When we are looking at cervical cancers, it is definitely one of the most common cancers. Most cervical cancers are caused by HPV, which is why the screenings are encouraged so that women get Pap-tested every three years.” She also recommended that women get regular Pap and HPV tests at the age of 30 and that parents get their sons and daughters vaccinated against HPV at ages 11 and 12. The spokeswoman for the Department of Health added that vaccinations are available through doctors’ offices or free at government health centres. She said: “The vaccine is part of the routine childhood schedule for immunization. HPV vaccination is important because once full immunity is reached, it can protect against the HPV viruses most likely to cause cervical cancer.” Because HPV is sexually transmitted, Ms Williams also urged people to use condoms to avoid contracting the virus, which is also linked to vaginal cancer in women and mouth, throat and penis cancers in men. Bermuda Cancer and Health Centre will highlight the disease and its prevention at a public meeting next week organized with the Ministry of Health as the island marks Cervical Cancer Awareness Month. Ms Williams said cervical cancer is the fourth most common cancer in women but added that there are no accurate figures for Bermuda because reporting is not mandatory. She added: “We’ve had several survivors. Looking at the death rate, it is highest in black women. “A lot of this is attributed to optimal healthcare. If women who are in lower income families or they don’t have adequate health insurance, they are not getting regularly checked and that’s when you tend to find cervical cancer, a lot of the times it’s advanced and it’s too late.” She added that all women are at risk, irrespective of race or ethnicity. Ms Williams said major symptoms, including abnormal vaginal bleeding, unusual vaginal discharge and pain during sex usually occur when the cancer is advanced. “If they catch it early, they have a higher survival rate, as is the case with any cancer. “Pap tests are so quick. There may be a little discomfort but it’s over and done with pretty quickly.” Ms Williams said other preventive measures include regular exercise, a healthy diet, quitting smoking and a reduction in alcohol consumption.
2018. January 18. Dr. Ewart Brown, owner of a clinic that is to discontinue its high-tech computerized X-ray service, turned up the heat yesterday on the Bermuda Health Council, which he blames for the closure of the service. Dr Brown, the former premier, said the end of CT scanning at the Brown-Darrell clinic could mean the loss of four jobs. He added the service at the Smith’s clinic would close at the end of the month because of a BHeC decision to cut fees. Dr Brown said the council, set up to monitor and improve island healthcare services, had been “functioning as a collection agency for the insurance companies”. He added that the decision was part of a sustained “political attack”. Dr Brown said the Brown-Darrell service complemented CT scanning available at the King Edward VII Memorial Hospital. “It’s been a very good arrangement, and for the same fee that the hospital has paid,” said Dr Brown. Dr Brown was flanked by Progressive Labour Party MPs and Jerome Lynch QC as he addressed a group of supporters outside the clinic. Mr Lynch said that there appeared to have been “some sort of targeting by the council”. He added that BHeC had cut diagnostic imaging fees “without any consultation”. Mr Lynch said: “Having come up with a figure, they decided to slash that even more.” New charges that came into effect last year has had a major effect on fees for CT imaging. Prices for one type of scan fell from $1,441 to $383, while another dropped from $1,543 to $542. Dr Brown said the BHeC had been put in place under a PLP government but that he had warned colleagues that “unless it is very carefully crafted, it’s going to be a problem”. He added: “Just as lawyers would not like it if a non-legal person were in charge of regulating them, doctors feel that those that regulate us should be doctors.” Dr Brown said several of BHeC’s proposals over the years had been “rejected by the public”. He highlighted a push for medical pre-certification, as well as tighter insurance regulations for mammograms, a proposal which was dropped after protests in June 2015. Dr Brown claimed BHeC had found the former One Bermuda Alliance administration to be one that “loved the idea of putting Dr Brown out of business”. He added his next steps were “a moving target” and that, while he hoped the Progressive Labour Party government would be able to work with him, he was “not here to try to tell them what to do”. The Ministry of Health said yesterday that a grant had been approved for service providers “in order to help ensure CT and MRI services are readily available to the public”. The grant was assigned to the Brown-Darrell Clinic, Bermuda Healthcare Services, also owned by Dr Brown, and the Bermuda Hospitals Board. The ministry said that the previous OBA administration’s cut in fees was “significantly” larger than the technical recommendation. A later statement from the ministry said: “The actual payments will be based on services provided, therefore the exact amounts for the period of operation will not be known until the end of the fiscal year. If the level of services remained the same as last year, Brown-Darrell and Bermuda Healthcare Services would receive approximately $778,000 and BHB $1.8 million. Bermuda currently has three CT scanners, placing us above the OECD average and among the highest in the world for CT scans per person.”
2017. December 15. Amendments increasing fees for health insurers were approved by the Senate. According to the Government, insurers did not object to the increases, which will help to fund the work of the Bermuda Health Council. The Health Insurance Amendment 2017, establishes a tiered fee structure for the renewal of approved health insurance schemes and the renewal of insurance licences. Both fees had previously been set at $1,000, the amendments set out a range of significantly higher rates based on gross premiums. The new fees will range from $12,500 in the lowest band, when annual gross revenue falls below $25 million, to $187,500 when annual gross premiums exceed $175 million. Crystal Caesar, starting the debate in the Senate, said the increase would go towards the BHC. She called the $1,000 fee “insufficient. Health insurance currently finances 62 per cent of all health system expenditure. The need to provide adequate and affordable health insurance coverage to all residents in Bermuda becomes more pronounced as the population ages and the incidence of chronic diseases increases. Within this context, the Bermuda Health Council has increased oversight focusing on areas of non-compliance and risks to the health system resulting from the business activities of health insurers and approved schemes. Regulatory oversight is especially important in the context of employers’ and public demand for more affordable health insurance premiums.” Ms Caesar added that the island’s health insurers were consulted about the increase and understood the reasoning for the change. She said: “The Bermuda Health Council held individual consultation meetings with all four insurers, two out of three approved schemes, the Association of Bermuda Insurers and Reinsurers, and the Association of Bermuda International Companies.
Stakeholders do not object to the proposed fee increases; they found the level and the logic of the fee increase acceptable assuming corresponding health insurance premium decreases, sustainable health system savings, and care delivery improvements. This amendment provides for licensing fees for health insurers and approved schemes to be aligned to the total premiums collected, with more rigorous scrutiny and onerous requirements applied where material amounts of business are transacted with respect to health insurance claims.” The legislation also expanded Mutual Reinsurance Fund Coverage by changing “haemodialysis” to “dialysis”, in a bid to fix what Ms Caesar said was an error. She told the Senate: “Covering all dialysis is crucial as research confirms that people with end-stage renal disease live longer and have more productive lives if they are able to access peritoneal dialysis before transplantation or starting haemodialysis. All dialysis was priced out of the Standard Health Benefit and into Mutual Reinsurance Fund. Therefore the premium to pay for both haemodialysis and peritoneal dialysis is being collected by the MRF, with no such funds in the SHB premium making it unaffordable for any insurance group with dialysis patients and, in particular, for HIP and FutureCare, which cover 80 per cent of all dialysis patients in Bermuda.” The Bermuda Health Council said it was “elated” by the passing of the amendment, saying that allowing MRF to cover dialysis will help to increase efficiency and reduce health costs. The BHC added the increase in licensing fees would help to improve regulatory oversight. Ricky Brathwaite, director of health economics, said the legislation as a “win” for the island’s healthcare system. Dr Brathwaite said: “The increased funds will be put towards improving quality care, standards and transparency in Bermuda’s health system.”
Authored,
researched, compiled and website-managed by Keith A. Forbes.
Multi-national © 2020. All Rights Reserved